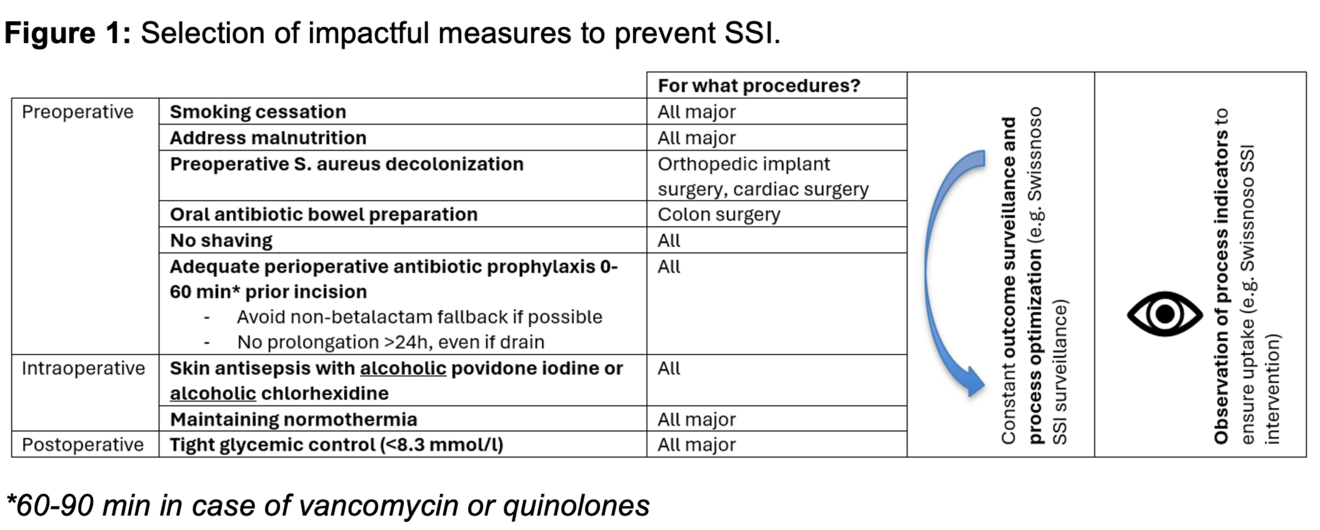
Surgical site infections (SSI) remain a major cause of postoperative morbidity, however, over half of the infections are preventable through evidence-based strategies. This review summarizes key measures applicable to the Swiss surgical setting, structured along the perioperative pathway.
Optimization of patient risk factors, namely preoperative smoking cessation, and screening for and targeting malnutrition are beneficial. In orthopedic implant surgery and cardiac surgery, preoperative Staphylococcus aureus decolonization strongly reduces the SSI risk. In colon surgery, oral antibiotic bowel preparation has shown strong protective effects. No shaving for hair removal should be used.
Perioperative antibiotic prophylaxis remains one of the most effective strategies, requiring precise timing and avoidance of unnecessary prolongation or fallback to non-betalactam options.
Highly effective intraoperative measures include skin antisepsis with alcohol-based solutions and maintenance of normothermia.
Postoperatively, strict glycemic control. Outcome surveillance (e.g. with Swissnoso SSI surveillance) with timely feedback and constant process optimization is crucial, and the uptake of the mentioned measures should be monitored, e.g. with Swissnoso SSI intervention module.
Introduction
Approximately 0.5% to 3% of patients undergoing surgery will experience infection of the surgical site,1 and surgical site infections (SSI) contribute with 20-40% to the whole of healthcare-associated infections (according to the Swissnoso point prevalence survey 2023). Clinically, SSI range from superficial incisional infections presenting with inflamation of the suture, to deep incisional (involving muscle/connective tissue ofth es incision) and to severe organ/space infections - including foreign-body, prosthetic implant-associated infections and sepsis. They are associated with increased length of hospital stay, reoperations and long-term disability. 2
The risk to endure a SSI is influenced by patient-related factors on the one hand: age, comorbidities such as diabetes mellitus, obesity, immunosuppression, malnutrition, carriage of S. aureus as well as smoking are known risk factors1. On the other hand, procedure-related factors such as emergency surgery with potential suboptimal patient preparation as well as complex surgery with longer procedure time increase the SSI risk1,3. Causative pathogens originate predominantly from the patient’s microbioma, with skin-colonizing microorganisms constituting the main source in most procedures.4 Commonly, procedures are stratified by the presence of microorganisms at the point of procedure according to the CDC Surgical Wound Classification scheme, with the risk of experiencing an organ space SSI increasing in clean/contaminated surgery 6-fold, in contaminated surgery 9-fold and in dirty surgery 18-fold compared to clean surgery5. Many prevention measures therefore aim to reduce the dislocation of microorganisms to sterile or semi-sterile compartiments of the body.
An estimated 55% of SSI are preventable6.
Good surgical technique is an indispensable base of prevention, as it minimizes the amount of avital tissue generated as well as influences procedure times. Nevertheless, as systematic process factors are strong influencers of the SSI risk, prevention requires a multimodal approach encompassing preoperative patient optimization, adherence to aseptic surgical technique, and standardized perioperative infection control measures. This review synthesizes the most relevant evidence-based strategies, emphasizing their applicability in the Swiss surgical context. Figure 1 gives an overview of the most impactful measures.
Measures to prevent SSI
1. Preoperative Measures
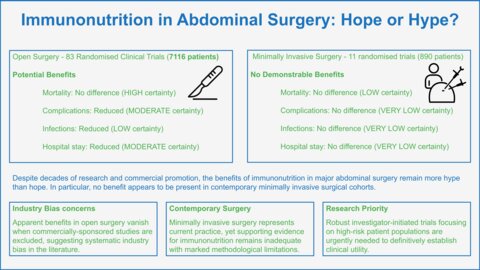
In elective surgery, the preoperative period may be used to optimize modifiable patient-related risk factors. Smoking cessation counseling and nicotine replacement therapy in smokers 6-8 weeks prior to surgery reduced infection rates from 23% to 4% in a Danish randomized controlled trial (RCT) in a high-risk orthopedic population7. Screening for and addressing malnutrition prior to major elective surgery, especially gastrointestinal surgery, is advisable: Preoperative isocaloric and isonitrogenous enteral nutrition support significantly reduce SSI in gastrointestinal surgery, as shown per a meta-analysis (RR 0.64, 95% CI 0.55-0.74)8. On the other hand, parenteral nutrition in the preoperative phase failed to confer a benefit in gastrointestinal and cardiac surgery patients9.
As mentioned, the skin microbioma is one of the main sources of causative pathogens. Showering or bathing with either soap or a disinfectant containing solution on the day of surgery or the preceding day is advised, based on the fact that it reduces the skin bacterial load; however, pre-operative-showering with chlorhexidine 4% prior to surgery did not significantly reduce SSI 10. Staphylococcus aureus is one of the main causative pathogens namely of implant-associated SSI.
Preoperative Staphylococcus aureus decolonization using nasal mupirocin and chlorhexidine skin washes 5 days prior surgery was demonstrated to be highly effective (RR 0.42, 95% CI 0.23-0.75) in a landmark trial11. The best effect was found in studies including mainly orthopedic implant surgery and cardiac surgery patients, and less or not detectable in RCTs including mainly general surgery, abdominal surgery or gynecology patients, where S. aureus is not the main contributor to SSI12. In daily practice, the patient process to screen patients and decolonize only in S. aureus colonized patients can be complicated and cumbersome. Therefore, the use of S. aureus decolonization without screening in all patients prior to undergoing orthopedic implant surgery or cardiac surgery (either implant surgery or sternotomy) is the preferred process by the authors. Skipping of nasal decontamination, thus limiting the decolonization procedure to disinfectant skin washes, results in lower effectiveness13.
A comparable reduction (to the mentioned decolonization) in SSI can be achieved in colon surgery by using oral antibiotic bowel preparation. Oral neomycin/metronidazole (OR 0.45, 95% CI 0.27-0.77), polymycin B/tobramycin (OR 0.48, 95% CI 0.30-0.76) and ciprofloxacin/metronidazole (OR 0.41, 95% CI 0.20-0.80) used one day before surgery are options supported by RCT data 14-18, ornidazole proved effective in an RCT19 with suboptimal perioperative prophylaxis; other oral antibiotic bowel preparation regimens such as paromomycin/metronidazole or rifaximin have only been associated with a lower SSI risk in observational studies 20 21.
Hair removal is indicated only when its presence interferes with the surgical procedure. In such cases, removal should be performed on the day of surgery using either clippers or a depilatory cream.22 Shaving should be strictly avoided, as it causes microinjuries to the skin and is associated with an increased risk of surgical site infections .23
Perioperative antibiotic prophylaxis is highly effective in preventing SSI in clean-contaminated, contaminated and dirty surgery, in clean surgery the number needed to prevent is generally only in a reasonable range in the case of implant surgery (in clean non-implant surgery an unreasonably large number of patients have to take prophylaxis to prevent an infection). Antibiotics should be administered 0-60 minutes prior incision (60-90 minutes in case of vancomycin or quinolones), as effectiveness is dependant on the timepoint of application; application after incision is associated with a higher SSI rate24. Whilst the benefit of intraoperative redosing remains uncertain, continuation over 24h is harmful25 and not associated with any benefit even in the presence of a drain26, with the sole possible exception in (ENT) free flap surgery. A Swissnoso sample guideline (https://swissnoso.ch/fileadmin/module/ssi_intervention/Dokumente_D/4_Sample_Guidelines/180816_Sample-Guideline_AMP_de.pdf) might be used as a blueprint for local perioperative prophylaxis guidelines, or freely available institutional prophylaxis guidelines such as https://antibiotika.insel.ch provide a detailed blueprint. Recent trial data suggests using prophylaxis also in low risk cholecystectomy27, and using a broader prophylactic spectrum such as piperacillin/tazobactam in high risk pancreatoduodenectomy28. Non-betalactam antibiotics are less preventive, and over 90% of reported penicillin allergies are not true allergies, therefore a fallback to non-betactam options in reported non-severe penicillin allergy should be avoided. The use of standardized surgical safety checklists is encouraged, and of particular importance in emergency surgery were processes tend to be less organized, thus, omitting of important process steps are more common 29.
2. Intraoperative Measures
Mainstay of intraoperative SSI prevention is skin antisepsis. For intact skin it should be performed with an alcohol-containing disinfectant with remanence, as water-based solutions are less protective30. In a recent Swiss multicenter RCT by the author of this overview, PVP-iodine in alcohol and chlorhexidine in alcohol proved to be equally effective excellent skin disinfectants31.
Avoiding hypothermia during surgery (with the exception of few specific indications) is crucial, as temperature monitoring and the use of measures such as forced air warming devices, active body surface warming devices, warming of infusion fluids to maintain normothermia <36°C reduces the SSI risk by a striking 2/332.
Coated sutures seem to be protective, however a large part of published studies suffer from conflict of interest33.
Surgeons and operating room stuffshould avoid transferring their own microbioma onto the surgical field. The use of sterile gowns, hair bouffants and surgical masks, surgical washing or hand disinfection as well as general sterile attire and well trained processes are a reasonable, historical established minimal standard - given the lack of high quality evidence its effect is somewhat difficult to quantify. Zoning concepts in OR tracts are reasonable, however not backed by high quality evidence. Unnecessary door openings are associated with increased SSI rates34.
The use of laminar airflow ventilation in ORs to prevent SSI has been debated35, however a recent Swiss study demonstrated an association of improved OR ventilation with lower rates at least in orthopedic and cardiac procedures36.
3. Postoperative Measures
As around 1/3 of surgical patients suffer from perioperative hyperglycemia, peri- and particularly postoperative tight glycemic control (monitoring and maintaining blood glucose below 8.3 mmol/l) reduces the SSI risk by over 1/3 – accordingly at least for major surgery a glucose control protocol should be implemented37.
Insicional wound irrigation with aqueous antiseptics is beneficial38. Sutures should be covered with sterile dressings39. Negative pressure would therapy seemed to reduce infections mainly in vascular and cardiac surgery in a meta-analysis40, whereas a recent RCT found no effect in laparotomy41, mirroring the findings of the mentioned meta-analysis not demonstrating a relevant benefit for abdominal, obstetric, orthopedic and plastic surgery40.
To continuously adapt the SSI prevention strategy, outcome surveillance e.g. with the Swissnoso SSI Surveillance module is recommended. To ensure the uptake of SSI prevention measures, we recommend using implementation bundles including process parameter observation, such as the Swissnoso SSI intervention module (https://swissnoso.ch/module/ssi-intervention/ueber-ssi-intervention/das-modul )
Surveillance itself is associated with a reduction of SSI rates42, nevertheless, feedback should be given in a timely manor in order to allow analysis of the effect of recent process changes and constant optimization of process factors.
Conclusion
Whilst surgical site infections are associated with increased length of hospital stay, reoperations and long-term disability, over half of them are preventable with a multimodal approach including perioperative process optimization. At least highly effective preventive measures such as S. aureus decolonization in orthopedic implant and cardiac surgery, gut decolonization in colon surgery, adequate antibiotic prophylaxis in the hour prior incision without continuation over 24h, avoidance of shaving as hair removal, skin antisepsis with alcoholic chlorhexidine or iodine, maintaining of normothermia and perioperative glycemic control should be implemented without gaps in Switzerland.
- Seidelman JL, Mantyh CR, Anderson DJ. Surgical Site Infection Prevention: A Review. JAMA. Jan 17 2023;329(3):244-252. doi:10.1001/jama.2022.24075
- Calderwood MS, Anderson DJ, Bratzler DW, et al. Strategies to prevent surgical site infections in acute-care hospitals: 2022 Update. Infect Control Hosp Epidemiol. May 2023;44(5):695-720. doi:10.1017/ice.2023.67
- Korol E, Johnston K, Waser N, et al. A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS One. 2013;8(12):e83743. doi:10.1371/journal.pone.0083743
- Wenzel RP. Surgical site infections and the microbiome: An updated perspective. Review. Infect Control Hosp Epidemiol. May 2019;40(5):590-596. doi: 10.1017/ice.2018.363. Epub 2019 Feb 21.
- Yin V, Cobb JP, Wightman SC, Atay SM, Harano T, Kim AW. Centers for Disease Control (CDC) Wound Classification is Prognostic of 30-Day Readmission Following Surgery. World J Surg. Oct 2023;47(10):2392-2400. doi:10.1007/s00268-023-07093-3
- Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. Feb 2011;32(2):101-14. doi:10.1086/657912
- Moller AM, Villebro N, Pedersen T, Tonnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet. Jan 12 2002;359(9301):114-7. doi:10.1016/S0140-6736(02)07369-5
- Marimuthu K, Varadhan KK, Ljungqvist O, Lobo DN. A meta-analysis of the effect of combinations of immune modulating nutrients on outcome in patients undergoing major open gastrointestinal surgery. Ann Surg. Jun 2012;255(6):1060-8. doi:10.1097/SLA.0b013e318252edf8
- Veterans Affairs Total Parenteral Nutrition Cooperative Study G. Perioperative total parenteral nutrition in surgical patients. N Engl J Med. Aug 22 1991;325(8):525-32. doi:10.1056/NEJM199108223250801
- Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. Feb 20 2015;2015(2):CD004985. doi:10.1002/14651858.CD004985.pub5
- Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. Jan 7 2010;362(1):9-17. doi:10.1056/NEJMoa0808939
- Perl TM, Cullen JJ, Wenzel RP, et al. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. N Engl J Med. Jun 13 2002;346(24):1871-7. doi:10.1056/NEJMoa003069
- Schweizer M, Perencevich E, McDanel J, et al. Effectiveness of a bundled intervention of decolonization and prophylaxis to decrease Gram positive surgical site infections after cardiac or orthopedic surgery: systematic review and meta-analysis. BMJ. Jun 13 2013;346:f2743. doi:10.1136/bmj.f2743
- Espin Basany E, Solis-Pena A, Pellino G, et al. Preoperative oral antibiotics and surgical-site infections in colon surgery (ORALEV): a multicentre, single-blind, pragmatic, randomised controlled trial. Lancet Gastroenterol Hepatol. Aug 2020;5(8):729-738. doi:10.1016/S2468-1253(20)30075-3
- Koskenvuo L, Lunkka P, Varpe P, et al. Morbidity After Mechanical Bowel Preparation and Oral Antibiotics Prior to Rectal Resection: The MOBILE2 Randomized Clinical Trial. JAMA Surg. Jun 1 2024;159(6):606-614. doi:10.1001/jamasurg.2024.0184
- Papp G, Saftics G, Szabo BE, et al. Systemic versus Oral and Systemic Antibiotic Prophylaxis (SOAP) study in colorectal surgery: prospective randomized multicentre trial. Br J Surg. Apr 5 2021;108(3):271-276. doi:10.1093/bjs/znaa131
- Abis GSA, Stockmann H, Bonjer HJ, et al. Randomized clinical trial of selective decontamination of the digestive tract in elective colorectal cancer surgery (SELECT trial). Br J Surg. Mar 2019;106(4):355-363. doi:10.1002/bjs.11117
- Roos D, Dijksman LM, Oudemans-van Straaten HM, de Wit LT, Gouma DJ, Gerhards MF. Randomized clinical trial of perioperative selective decontamination of the digestive tract versus placebo in elective gastrointestinal surgery. Br J Surg. Oct 2011;98(10):1365-72. doi:10.1002/bjs.7631
- Futier E, Jaber S, Garot M, et al. Effect of oral antimicrobial prophylaxis on surgical site infection after elective colorectal surgery: multicentre, randomised, double blind, placebo controlled trial. BMJ. Nov 3 2022;379:e071476. doi:10.1136/bmj-2022-071476
- Mehdorn M, Lubbert C, Chaberny IF, Gockel I, Jansen-Winkeln B. Mechanical plus oral bowel preparation with paromomycin and metronidazole reduces infectious complications in elective colorectal surgery: a matched case-control study. Int J Colorectal Dis. Sep 2021;36(9):1839-1849. doi:10.1007/s00384-021-03931-9
- Yoon SH, Yang IJ, Kim JY, Lee KH. Efficacy of a 1 day Rifaximin and Metronidazole Regimen and Mechanical Bowel Preparation for Preventing Surgical Site Infection in Minimally Invasive Colorectal Cancer Surgery: A Prospective Observational Study. Am Surg. Apr 2024;90(4):550-559. doi:10.1177/00031348231200667
- Alexander JW, Fischer JE, Boyajian M, Palmquist J, Morris MJ. The influence of hair-removal methods on wound infections. Arch Surg. Mar 1983;118(3):347-52. doi:10.1001/archsurg.1983.01390030079013
- Tanner J, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. Aug 26 2021;8(8):CD004122. doi:10.1002/14651858.CD004122.pub5
- van Kasteren ME, Mannien J, Ott A, Kullberg BJ, de Boer AS, Gyssens IC. Antibiotic prophylaxis and the risk of surgical site infections following total hip arthroplasty: timely administration is the most important factor. Clin Infect Dis. Apr 1 2007;44(7):921-7. doi:10.1086/512192
- Branch-Elliman W, O'Brien W, Strymish J, Itani K, Wyatt C, Gupta K. Association of Duration and Type of Surgical Prophylaxis With Antimicrobial-Associated Adverse Events. JAMA Surg. Jul 1 2019;154(7):590-598. doi:10.1001/jamasurg.2019.0569
- Berrios-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. May 03 2017;doi:10.1001/jamasurg.2017.0904
- van Braak WG, Ponten JEH, Loozen CS, et al. Antibiotic prophylaxis for acute cholecystectomy: PEANUTS II multicentre randomized non-inferiority clinical trial. Br J Surg. Feb 24 2022;109(3):267-273. doi:10.1093/bjs/znab441
- D'Angelica MI, Ellis RJ, Liu JB, et al. Piperacillin-Tazobactam Compared With Cefoxitin as Antimicrobial Prophylaxis for Pancreatoduodenectomy: A Randomized Clinical Trial. JAMA. May 9 2023;329(18):1579-1588. doi:10.1001/jama.2023.5728
- van Klei WA, Hoff RG, van Aarnhem EE, et al. Effects of the introduction of the WHO "Surgical Safety Checklist" on in-hospital mortality: a cohort study. Ann Surg. Jan 2012;255(1):44-9. doi:10.1097/SLA.0b013e31823779ae
- Darouiche RO, Wall MJ, Jr., Itani KM, et al. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N Engl J Med. Jan 7 2010;362(1):18-26. doi:10.1056/NEJMoa0810988
- Widmer AF, Atkinson A, Kuster SP, et al. Povidone Iodine vs Chlorhexidine Gluconate in Alcohol for Preoperative Skin Antisepsis: A Randomized Clinical Trial. JAMA. Aug 20 2024;332(7):541-549. doi:10.1001/jama.2024.8531
- Madrid E, Urrutia G, Roque i Figuls M, et al. Active body surface warming systems for preventing complications caused by inadvertent perioperative hypothermia in adults. Cochrane Database Syst Rev. Apr 21 2016;4(4):CD009016. doi:10.1002/14651858.CD009016.pub2
- Yang Y, Zhou Z, Ma R, Ren J, Wu X. Antimicrobial-coated sutures versus non-coated sutures in reducing surgical site infection: an updated systematic review and meta-analysis. J Hosp Infect. Aug 2024;150:40-50. doi:10.1016/j.jhin.2024.04.027
- Groenen H, Jalalzadeh H, Bontekoning N, et al. Effect of the number of door openings in the operating room on surgical site infections: individual-patient data meta-analysis. BJS Open. May 7 2025;9(3)doi:10.1093/bjsopen/zraf044
- Bischoff P, Kubilay NZ, Allegranzi B, Egger M, Gastmeier P. Effect of laminar airflow ventilation on surgical site infections: a systematic review and meta-analysis. Lancet Infect Dis. May 2017;17(5):553-561. doi:10.1016/S1473-3099(17)30059-2
- Surial B, Atkinson A, Kulpmann R, et al. Better Operating Room Ventilation as Determined by a Novel Ventilation Index is Associated With Lower Rates of Surgical Site Infections. Ann Surg. Nov 1 2022;276(5):e353-e360. doi:10.1097/SLA.0000000000005670
- Wang YY, Hu SF, Ying HM, et al. Postoperative tight glycemic control significantly reduces postoperative infection rates in patients undergoing surgery: a meta-analysis. BMC Endocr Disord. Jun 22 2018;18(1):42. doi:10.1186/s12902-018-0268-9
- Groenen H, Bontekoning N, Jalalzadeh H, et al. Incisional Wound Irrigation for the Prevention of Surgical Site Infection: A Systematic Review and Network Meta-Analysis. JAMA Surg. Jul 1 2024;159(7):792-800. doi:10.1001/jamasurg.2024.0775
- Global Guidelines for the Prevention of Surgical Site Infection. 2016. WHO Guidelines.
- Zwanenburg PR, Tol BT, Obdeijn MC, Lapid O, Gans SL, Boermeester MA. Meta-analysis, Meta-regression, and GRADE Assessment of Randomized and Nonrandomized Studies of Incisional Negative Pressure Wound Therapy Versus Control Dressings for the Prevention of Postoperative Wound Complications. Ann Surg. Jul 2020;272(1):81-91. doi:10.1097/SLA.0000000000003644
- Group STS, Atherton K, Brown J, et al. Negative Pressure Dressings to Prevent Surgical Site Infection After Emergency Laparotomy: The SUNRRISE Randomized Clinical Trial. JAMA. Mar 11 2025;333(10):853-863. doi:10.1001/jama.2024.24764
- Haley RW, Culver DH, White JW, et al. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am J Epidemiol. Feb 1985;121(2):182-205. doi:10.1093/oxfordjournals.aje.a113990