ERAS originated in the 1990s, from the groundbreaking work of Professor Henrik Kehlet, a Danish surgeon and physiologist, whose research laid the scientific foundation for an internationally recognized standard of perioperative care [1]. He focused on the physiological and metabolic responses to surgical trauma and methods to reduce the adverse systemic effects [1]. Kehlet’s work showed that these perioperative care pathways could potentially reduce physiological insults, thereby reducing complications, accelerating recovery, and improving outcomes [2].
This led to the development of the Fast Track Surgery concept, which is an evidence-based approach that can be applied in the preoperative, intraoperative, and postoperative care [3,4]. In 2001, it evolved into ERAS via collaborative international protocols [5]. The ERAS Society, founded in 2010 in Stockholm, Sweden, enabled global multidisciplinary collaboration among surgeons and researchers [6]. Since then, ERAS guidelines have developed and expanded across multiple surgical specialties, including gynecologic, urologic, hepatobiliary, esophageal, and bariatric surgery [7–13]. A key feature is its data-driven quality improvement process, supported by the ERAS Interactive Audit System (EIAS), a global registry that enables benchmarking of compliance and outcomes.
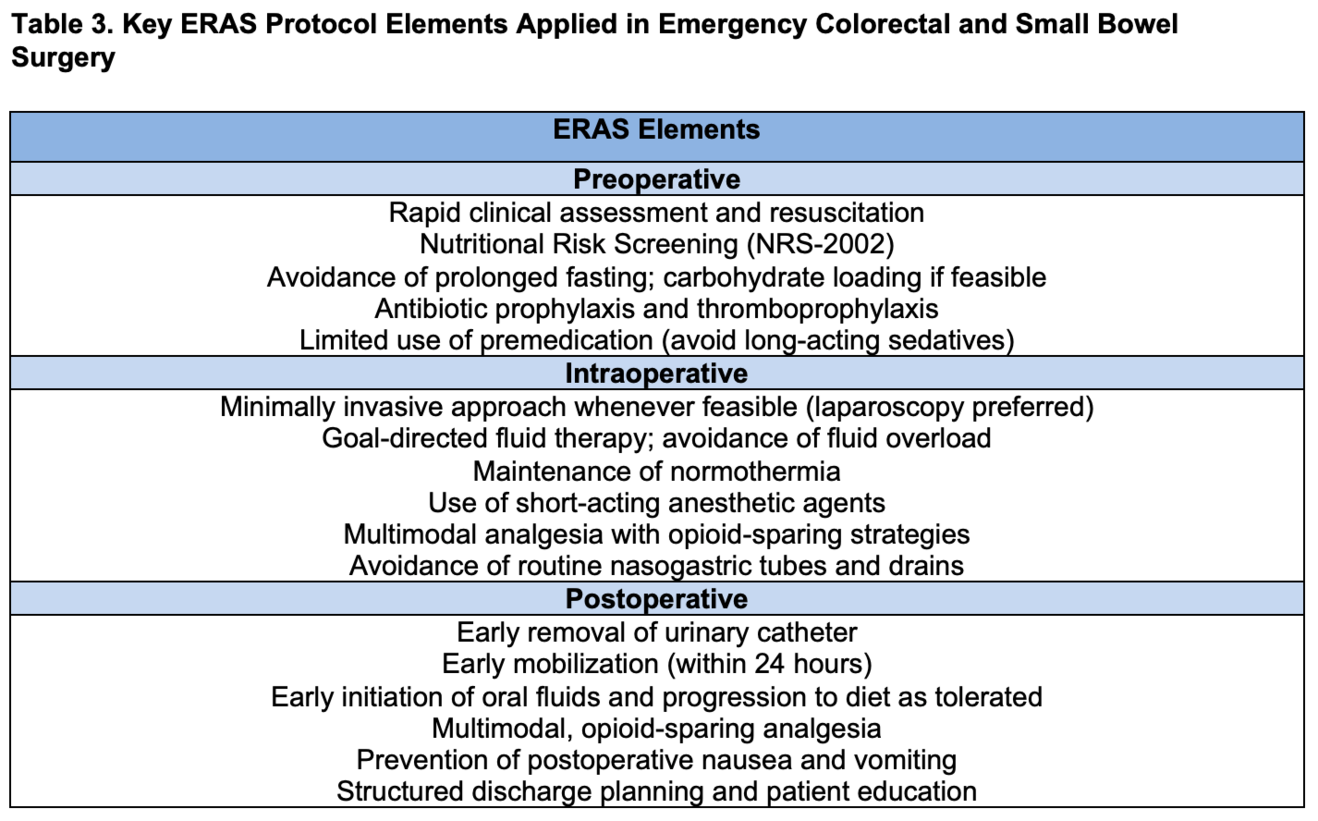
In colorectal surgery, the recent update of the ERAS guidelines was completed in 2018 and published in 2019 [10]. The protocols include evidence-based recommendations for a number of principles, including early oral nutrition initiation, minimally invasive surgical techniques, and opioid-sparing analgesia [10].
High ERAS protocol compliance has been clearly linked to better patient outcomes, such as fewer postoperative complications, shorter hospital stays, and higher levels of overall patient satisfaction [14, 15]. Even though ERAS is widely used in elective surgeries, emergency procedures are still difficult because of time constraints, case instability, and inadequate preoperative planning [16]. The literature lacks explicit ERAS guidelines for these situations, even though 30% of colorectal surgeries are emergencies [17]. Nevertheless, mounting data indicates that even a small amount of ERAS adherence during emergency surgery greatly improves recovery and lowers complications.
Methods
Study design and setting
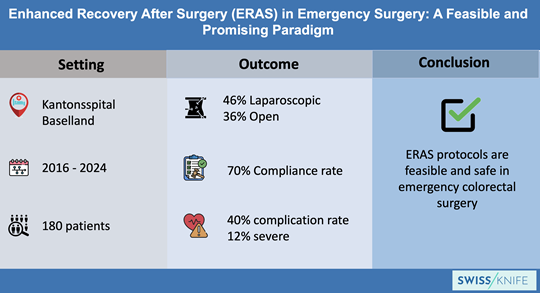
This retrospective observational cohort study was conducted at the Kantonsspital Baselland, Switzerland. From May 2016 to the end of October 2024, all colorectal surgeries performed in the emergency settings were documented and entered into the ERAS Interactive Audit System (EIAS) database.
All consecutive adult patients (≥18 years) undergoing emergency colorectal surgery during the study period were screened for inclusion. Emergency surgeries were stratified to three subgroups: emergency surgery (<2 hours), acute surgery (2-24 hours), and surgery after unplanned admission.
Data collection
Data were extracted from the ERAS Interactive Audit System (EIAS) and the hospital records, including patient demographics, comorbidities, preoperative status, operative details, ERAS compliance, and postoperative outcomes.
Outcomes
The primary outcome was the overall compliance to the protocol and the components (demonstrated in Table 3), while secondary outcomes included length of stay, complication rates, anastomotic leakage, discharge destination, and 30-day mortality.
Statistical analysis
Continuous variables were reported as mean ± SD or median (IQR) and categorical variables as counts and percentages; group comparisons were performed using χ² or Fisher’s exact test for categorical data and Student’s t-test or Mann–Whitney U test for continuous data, with p < 0.05 considered statistically significant.
Results
Of these cases, 180 operations were classified as emergency interventions, reflecting the hospital’s commitment to integrating ERAS principles even in acute care scenarios.
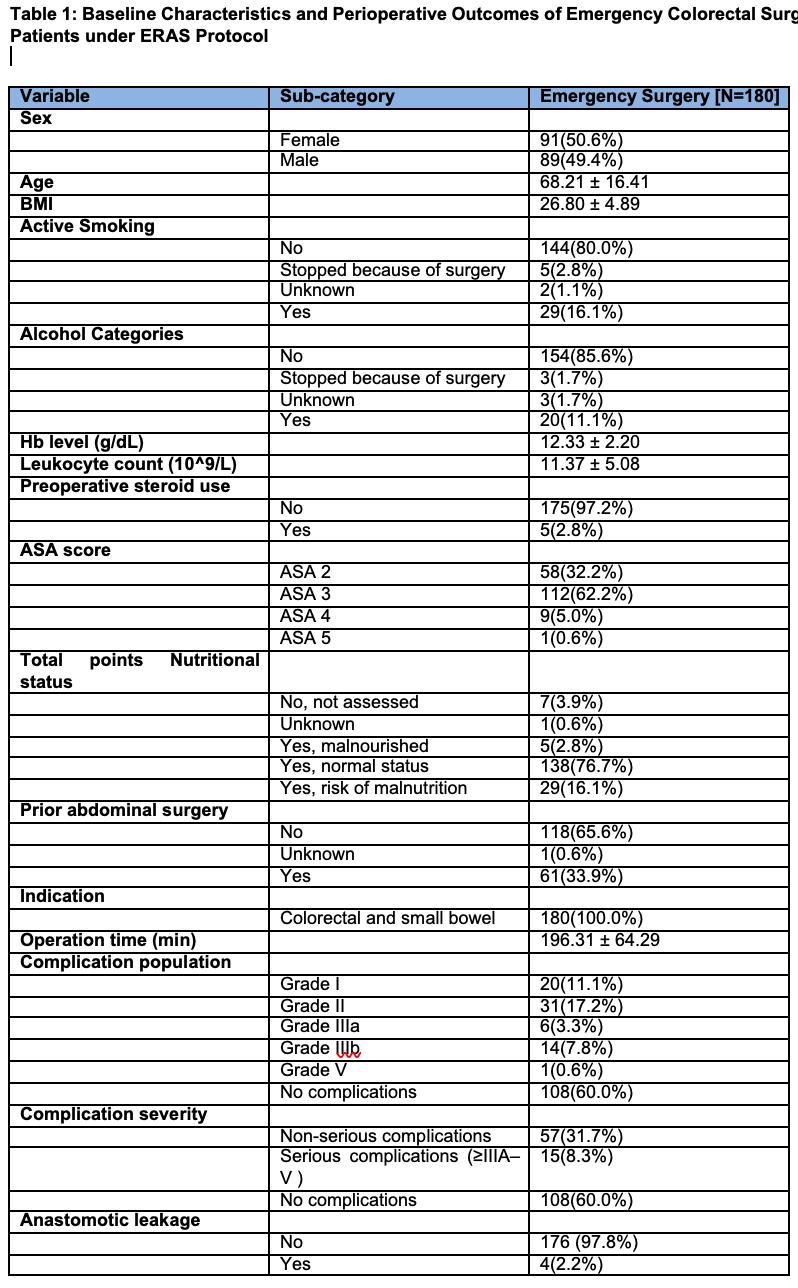
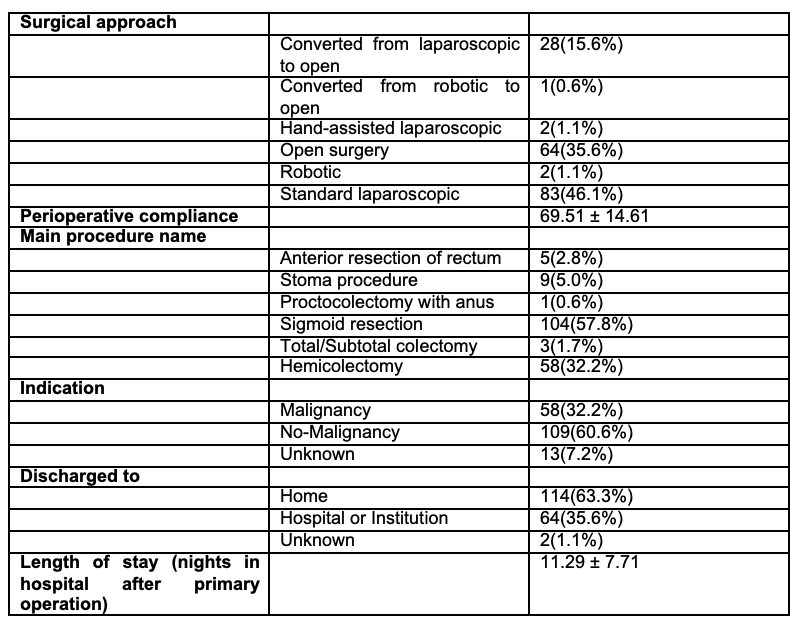
Whenever clinically feasible and logistically appropriate, the ERAS protocol elements were applied to patients undergoing emergency colorectal or small bowel surgeries. It should be emphasized, however, that patients anticipated to require prolonged mechanical ventilation postoperatively in the intensive care unit (ICU)—typically beyond several days—were systematically excluded from the dataset to ensure a focused evaluation of ERAS adherence. The corresponding patient statistics are detailed in Table 1, which outlines the demographic, surgical, and clinical characteristics of the included cohort.
Preoperative Characteristics
Among the 180 patients who underwent emergency surgical procedures under the ERAS framework, the sex distribution was nearly balanced, with 50.6% identified as female and 49.4% as male. The mean age of the cohort was 68.21 ± 16.41, signifying a predominantly geriatric population. The mean body mass index (BMI) was measured at 26.80 ± 4.89 kg/m², a value that places the average patient within the overweight range according to standard classification systems.
Preoperatively, 16.1% of the patients disclosed active smoking, while 11.1% reported ongoing alcohol consumption. Malnutrition or risk thereof was identified in 18.9% of individuals based on nutritional screening tools such as Nutritional Risk Scenting Tool and Malnutrition Universal Screening Tool. Baseline laboratory values showed an average hemoglobin concentration of 12.33 ± 2.20 g/dL, and leukocyte counts were elevated at 11.37 ± 5.08 x10⁹/L, suggestive of an ongoing systemic inflammatory state.
In terms of overall physical status, most patients were designated as ASA III (62.2%), reflecting the presence of significant systemic disease, while 5.6% were classified as ASA IV or V, denoting more critical baseline health status. Additionally, 33.9% had a history of previous abdominal surgery, a relevant risk factor in emergent operative contexts.
Surgical Procedures and Technique
The most frequently performed emergency procedures included sigmoid resections, accounting for 57.8% of operations, followed by hemicolectomies (32.2%) and stoma procedures (5.0%). The mean operative time for these procedures was 196.31 ± 64.29 minutes, demonstrating the complexity and duration of emergency colorectal surgeries.
The choice of surgical approach was guided primarily by feasibility and patient safety considerations. In accordance with ERAS principles, a minimally invasive approach (laparoscopic or hand-assisted laparoscopic) was preferred whenever technically achievable and clinically appropriate. Open surgery was performed in cases where laparoscopy was not deemed feasible or safe at the outset. Intraoperative conversion from minimally invasive to open surgery was undertaken in situations of technical difficulty, such as dense adhesions or unfavorable anatomy, or when patient instability necessitated a more expeditious approach.
Regarding surgical approach, 46.1% of operations were completed using a standard laparoscopic approach, 1.1% using a hand-assisted laparoscopic approach (combined 47.2%), while 35.6% were performed through open surgery. In 15.6% of cases, an intraoperative conversion from a minimally invasive technique to an open procedure was necessary, typically due to technical difficulty or patient instability.
Anastomosis formation was achieved in a considerable proportion of patients: 45.0% underwent colorectal anastomosis, while 22.2% received small bowel–colon anastomoses. The rate of anastomotic leakage was relatively low at 2.2%. Notably, all cases of leakage required surgical re-intervention; no patients were managed non-operatively through percutaneous drainage or conservative therapy.
ERAS Protocol Compliance
Adherence to ERAS protocol elements was assessed in both the preoperative and perioperative phases. The average compliance was 69.51 ± 14.61%. These metrics illustrate the practicality and success of ERAS implementation even within the unpredictable environment of emergency surgery.
Postoperative Outcomes and Complications
The mean length of hospital stay following the emergency cases was 11.29 ± 7.71 days. Upon discharge, 63.3% of patients were able to return directly home, while 35.6% required ongoing care in either a hospital or institutional setting, reflecting varying levels of functional recovery.
Postoperative morbidity was reported in 40.0% of emergency cases, with the majority of complications graded as Clavien-Dindo I (11.1%) or II (17.2%), indicating minor severity. Serious complications (Grade IIIa–V) occurred in 11.7% of the cohort.
Specific complications included pulmonary events in 5.6%, gastrointestinal complications in 15.6%, and cardiac events in 2.8%. Wound complications presented in only 4.4% of patients, underscoring the potential impact of contaminated fields and emergent surgical timing. Other complications—such as those affecting the renal system, central nervous system (CNS), or resulting in thromboembolic phenomena—were rare.
Subgroups
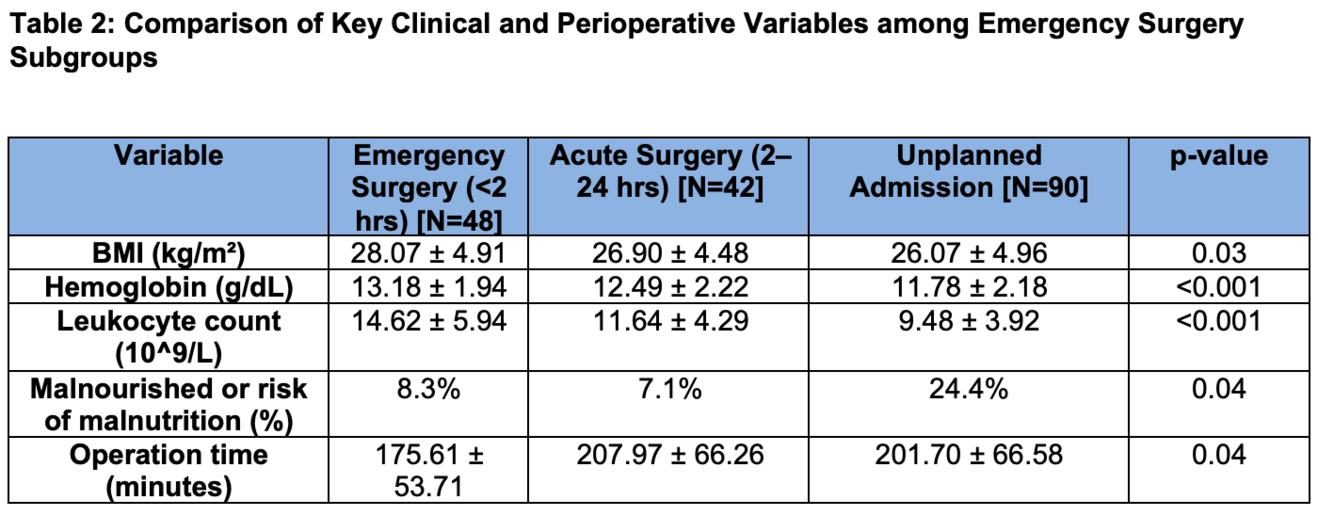
The patients were further subdivided into three emergency surgery categories: emergency surgery (<2 hours), acute surgery (2–24 hours), and surgery after unplanned admission (admission that was not scheduled in advance and occurred due to an unexpected clinical deterioration); several statistically significant differences were observed and are demonstrated in Table 2. Regarding nutritional status, patients undergoing surgery after unplanned admission had a higher proportion of malnutrition or nutritional risk (24.4%) than those in the acute (7.1%) and emergency (8.3%) groups, with a p-value of 0.036. Operation time was the shortest in the emergency surgery group (175.61 ± 53.71 mins) versus the acute (207.97 ± 66.26 mins) and unplanned admission (201.70 ± 66.58 mins), p = 0.039. There were no statistically significant differences in other factors such as complication rates or anastomotic leakage.
Discussion
The findings from our institutional cohort strongly demonstrate that the principles of Enhanced Recovery After Surgery (ERAS) are feasibly implemented but also effectively translated into meaningful clinical outcomes within the high-pressure context of emergency surgical care. Despite the well-documented high-risk profile of patients undergoing emergency colorectal or small bowel surgery—characterized by factors such as advanced age, higher ASA physical status classifications, ongoing systemic inflammation, and frequent comorbidities—our data indicate that perioperative outcomes remained both acceptable and clinically favorable.
A particularly noteworthy observation was our ability to maintain relatively high compliance with intraoperative and postoperative ERAS elements, achieving an average adherence rate of approximately 69%, which is consistent with or even exceeds benchmarks in many elective surgical settings. [18-19] This level of consistency indicates that even in time-sensitive, resource-constrained, and unpredictable clinical scenarios, it is possible to deliver structured, protocol-driven perioperative care. The core components of ERAS—such as early mobilization, careful fluid management to avoid overload, prompt reintroduction of oral nutrition, and multimodal analgesia- are foundational to improved recovery and likely played an important role in the outcomes observed in our cohort.
Full compliance with every ERAS element may not be necessary to derive clinical benefit. This observation highlights the importance of institutional readiness, including having trained ERAS coordinators, adaptable clinical workflows, and multidisciplinary cooperation, which are essential to maintain protocol fidelity during emergency admissions.
Our results align with findings from the wider literature. For example, Roulin et al. (2014) demonstrated in a prospective study of emergency colon resections that ERAS compliance was 77% in elective cases versus 57% in emergency settings [18]. Postoperative compliance was also lower in emergency patients (49% compared to 67%), largely due to the lack of preoperative preparation. After applying the ERAS protocol to emergency surgeries, Bisagni et al.'s study revealed a 50% postoperative compliance rate [19]. They saw notable improvements despite lower compliance: overall morbidity and mortality stayed the same, hospital stays decreased, and the use of laparoscopic procedures increased from 12% to 40%. Additionally, the ERAS implementation resulted in cost savings of over €1,000 per patient, demonstrating the approach's additional economic value [19].
With respect to postoperative complications, our results fall within a clinically acceptable range for emergency surgical populations. The overall complication rate was 40%, yet the majority of these events were minor, falling into Clavien-Dindo Grade I or II categories. Only 8.3% of patients experienced serious complications (Clavien-Dindo IIIb-V), and the rate of anastomotic leakage was 2.2%, a figure that remains low in comparison to the current data on emergency colorectal surgery, which can reach up to a 30% rate [20-21]. Importantly, all the anastomotic leakage cases in our study were treated surgically, thereby reflecting an appropriate and adequate clinical judgment in the postoperative period. Decisions regarding whether to proceed with primary anastomosis or consider fecal diversion were made with several factors in mind, such as the intraoperative and physiological factors, aligning with the risk-adapted approach to ERAS principles.
Our results were promising in terms of functional recovery; over 60% of patients were discharged home directly, which is a strong indicator of complete recovery. This finding is especially significant given the population's comorbidity and advanced age. The median hospital length of stay, just over 11 days, is well within reason when accounting for the emergent nature of the procedures and the postoperative recovery demands.
Among the most commonly observed complications were pulmonary, gastrointestinal, and wound-related events. Although wound complications were significant in our analysis, their overall incidence was 4.4%, which is relatively low compared with control groups reported in the literature, where rates range from 3% to 17.8% [22-24]. This outcome likely reflects the contaminated surgical fields, limited preoperative optimization, and the urgency with which many procedures had to be undertaken. Nonetheless, these complications did not appear to significantly affect the overall hospital stay or postoperative mortality, reaffirming the resilience of the ERAS framework in such contexts.
Additional evidence comes from randomized trials. For instance, Pranavi et al. showed that an adapted ERAS protocol in patients with peritonitis resulted in shortened hospital stays, quicker bowel recovery, and lower wound infection rates compared to the standard care [25]. Aggarwal et al. supported these results, with findings significant for fewer reinsertions of nasogastric tubes, as well as similar safety outcomes in emergency laparotomy patients managed with a modified ERAS protocol [26]. Multiple meta-analyses further add to the notion that ERAS use in emergency surgery leads to faster return of bowel function and reduced surgical site infection rates, without increasing 30-day mortality, reoperation, or readmission rates [24-25].
The limited window for implementing preoperative protocols is the primary obstacle when applying ERAS protocols to emergency surgery. Preoperative ERAS elements cannot be meaningfully implemented in many patients due to the urgency of the surgical indication, which is frequently life-threatening due to sepsis, perforation, or obstruction. Between 2021 and 2023, the ERAS Society released three sections of Guidelines for Perioperative Care in Emergency Laparotomy in acknowledgment of this limitation [27–31]. With the exception of trauma, vascular, appendectomy, and cholecystectomy cases, these guidelines offer systematic, evidence-based recommendations for non-elective procedures that address life-threatening intra-abdominal pathologies.
Crucially, extensive programs such as England's National Emergency Laparotomy Audit (NELA) have demonstrated quantifiable success, as evidenced by the 30-day mortality rate dropping from 11.8% to 9.3% since its inception in 2013 [32]. These outcomes highlight the effectiveness of structured, protocolized perioperative care models and support their ongoing adoption.
The majority of ERAS components can still be pursued and adapted, even under emergency conditions. While full compliance may be unachievable in many cases, the core philosophy of ERAS—multidisciplinary coordination, patient-centered care, and evidence-based interventions—remains relevant. Clinicians must recognize that even frail and critically ill patients can benefit from structured, thoughtful perioperative protocols. The focus should not be solely on hitting high compliance scores but rather on using available resources effectively to guide patients through this vulnerable period. When viewed through this lens, the ERAS framework emerges not only as applicable but as a clinically sensible and ethically sound model for modern emergency surgical care.
Conclusion
The implementation of the ERAS protocol in the context of emergency colorectal and small bowel surgery has proven not only to be practically feasible but also clinically advantageous. Our institutional experience at Kantonsspital Baselland provides compelling evidence that, even under challenging conditions typically associated with emergency surgical care—such as limited preoperative optimization, greater physiological instability, and increased patient comorbidity burden—ERAS pathways can still be effectively integrated into the care continuum. In summary, our data advocate for the routine integration of ERAS protocols into acute surgical care pathways, reflecting a broader shift toward standardized, high-quality perioperative management in emergency settings. This approach not only enhances patient outcomes but also promotes consistency, safety, and efficiency across varying clinical environments.
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183(6):630-641.
- Holte, K., P. Jensen, and H. Kehlet, Physiologic effects of intravenous fluid administration in healthy volunteers. Anesth Analg, 2003. 96(5): p. 1504-9, table of contents.
- Delaney, C.P., et al., 'Fast track' postoperative management protocol for patients with high co-morbidity undergoing complex abdominal and pelvic colorectal surgery. Br J Surg, 2001. 88(11): p. 1533-8.
- Wilmore, D.W. and H. Kehlet, Management of patients in fast track surgery. BMJ, 2001. 322(7284): p. 473-6.
- Fearon, K.C., et al., Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr, 2005. 24(3): p. 466-77.
- Society, E. Geschichte von ERAS. [ONLINE] 2021]; Available from: https://erassociety.org/about/history/.
- Feldheiser, A., et al., Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand, 2016. 60(3): p. 289-334.
- Thorell, A., et al., Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg, 2016. 40(9): p. 2065-83.
- Gustafsson, U.O., et al., Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr, 2012. 31(6): p. 783-800.
- Gustafsson, U.O., et al., Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS((R))) Society Recommendations: 2018. World J Surg, 2019. 43(3): p. 659-695.
- Francis, N., et al., Manual of fast track recovery for colorectal surgery. 2012: Springer Science & Business Media.
- Feldman, L.S., et al., The SAGES/ERAS® Society manual of enhanced recovery programs for gastrointestinal surgery. 2015: Springer.
- Lassen, K., et al., Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg, 2009. 144(10): p. 961-9.
- Arrick, L., et al., Enhanced recovery after surgery in colorectal surgery: Impact of protocol adherence on patient outcomes. J Clin Anesth, 2019. 55: p. 7-12.
- Turaga, A. H. (2023). Enhanced Recovery After Surgery (ERAS) protocols for improving outcomes for patients undergoing major colorectal surgery. Cureus, 15(7), e41755. https://doi.org/10.7759/cureus.41755
- Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer. Medicine. 2018 Sep;97(39):e12348.
- Lohsiriwat V, Jitmungngan R. Enhanced recovery after surgery in emergency colorectal surgery: Review of literature and current practices. World Journal of Gastrointestinal Surgery. 2019 Feb 27;11(2):41–52.
- Roulin, D., et al., Enhanced recovery pathway for urgent colectomy. World J Surg, 2014. 38(8): p. 2153-9.
- Bisagni, P., et al., Cost saving in implementing ERAS protocol in emergency abdominal surgery. BMC Surg, 2024. 24(1): p. 70.
- He, J., He, M., Tang, JH. et al. Anastomotic leak risk factors following colon cancer resection: a systematic review and meta-analysis. Langenbecks Arch Surg 408, 252 (2023).
- Altınlı, E., et al., Evaluation of Factors Associated with Anastomotic Leakage in Colorectal Surgery. Turk J Colorectal Dis, 2018. 28(4): p. 129–135.
- Ikeda, A., Fukunaga, Y., Akiyoshi, T. et al. Wound infection in colorectal cancer resections through a laparoscopic approach: a single-center prospective observational study of over 3000 cases. Discov Onc 12, 2 (2021). https://doi.org/10.1007/s12672-021-00396-8
- Al-Amry, A. L., Obadiel, Y. A., Al-Shehari, M. M., Gailan, W. M., Bajubair, M. H., & Jowah, H. M. (2024). Early Postoperative Complications in Colorectal Cancer Patients Following Colorectal Surgery Among Yemeni Patients: A Prospective Study. Open Access Surgery, 17, 81–90. https://doi.org/10.2147/OAS.S465936
- Kirchhoff P, Clavien PA, Hahnloser D. Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg. 2010 Mar 25;4(1):5. doi: 10.1186/1754-9493-4-5
- Pranavi, A.R., et al., Adapted ERAS Pathway Versus Standard Care in Patients Undergoing Emergency Surgery for Perforation Peritonitis-a Randomized Controlled Trial. J Gastrointest Surg, 2022. 26(1): p. 39-49.
- Aggarwal, A., et al., Modified Enhanced Recovery After Surgery (ERAS) Protocol Versus Non-ERAS Protocol in Patients Undergoing Emergency Laparotomy for Acute Intestinal Obstruction: A Randomized Controlled Trial. World J Surg, 2023. 47(12): p. 2990-2999.
- Hajibandeh, S., et al., Meta-analysis of Enhanced Recovery After Surgery (ERAS) Protocols in Emergency Abdominal Surgery. World J Surg, 2020. 44(5): p. 1336-1348.
- Ahmed, A., et al., Efficacy of Enhanced Recovery After Surgery (ERAS) Protocols in Emergency Colorectal Surgery: A Meta-Analytical Comparison With Conventional Care in Terms of Outcomes and Complications. Cureus, 2024. 16(10): p. E71630.
- Peden, C.J., et al., Guidelines for Perioperative Care for Emergency Laparotomy Enhanced Recovery After Surgery (ERAS) Society Recommendations: Part 1-Preoperative: Diagnosis, Rapid Assessment and Optimization. World J Surg, 2021. 45(5): p. 1272-1290.
- Scott, M.J., et al., Consensus Guidelines for Perioperative Care for Emergency Laparotomy Enhanced Recovery After Surgery (ERAS((R))) Society Recommendations Part 2-Emergency Laparotomy: Intra- and Postoperative Care. World J Surg, 2023. 47(8): p. 1850-1880.
- Peden, C.J., et al., Enhanced Recovery After Surgery (ERAS(R)) Society Consensus Guidelines for Emergency Laparotomy Part 3: Organizational Aspects and General Considerations for Management of the Emergency Laparotomy Patient. World J Surg, 2023. 47(8): p. 1881-1898.
- NELA Project Team (2019) Fifth Patient Report of the National Emergency Laparotomy Audit. 2019 25.07.2025]