Precision medicine offers personalized and targeted treatment strategies in healthcare. However, the roadmap to realizing precision medicine remains largely unclear. There are multiple challenges in today’s healthcare environment, such as optimal collaboration among various disciplines, organizations in networks versus centralization efforts, digital transformation, process efficiency, quality issues and costs.
Implementing precision medicine requires a systematic approach and the integration of various components. By following the roadmap as presented herein, healthcare professionals can enhance care quality, optimize patient outcomes, and provide personalized treatment plans. The integration of data-driven methodologies and the development of the patient digital twin hold great promise for improved patient experiences and better long-term outcomes in medical care.
Surgeons historically played a pivotal role in driving medical innovations, with their advancements subsequently being adopted across the field of medicine. In case of sarcoma surgery, a multidisciplinary and intricate approach is essential to achieve optimal outcomes. The collaboration and coordination of various disciplines are crucial not only for surgical procedures but for all aspects of sarcoma care. This integrated approach holds immense significance in defining precision medicine. By embracing a comprehensive team-based approach, the transdisciplinary sarcoma surgery-based philosophy can pave the way for advancements in the overall care and treatment of sarcoma patients, pushing the boundaries of what is currently possible. The innovations and breakthroughs emerging from sarcoma surgery may set the stage for the next level of development in sarcoma care, benefiting patients by providing more precise and effective interventions and care.
The SwissSarcomaNetwork (SSN) focuses on the sustainable health care triad and specifically on the quality of sarcoma care. This article aims to provide a concise roadmap for implementing precision medicine, addressing the main goal of providing personalized treatment. For each step of the roadmap, a brief note is included on the current SSN achievements.
1. Start of the process
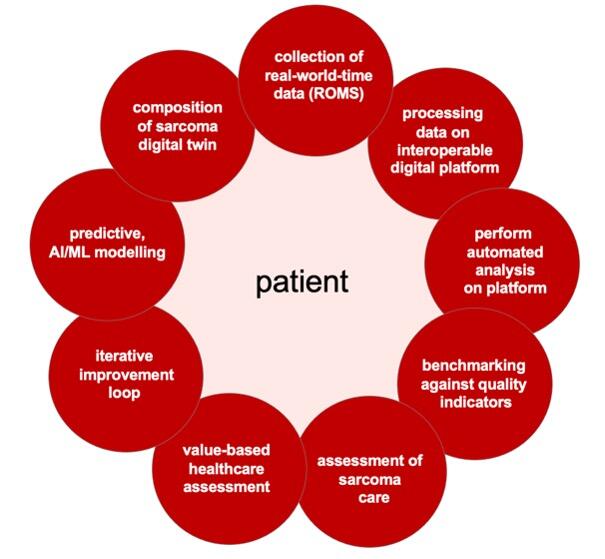
The journey to enhance sarcoma care begins by recognizing the importance of data-driven approaches and adopting a systematic methodology. Multidisciplinary teams comprising healthcare professionals, data scientists, and technology experts collaborate to develop a comprehensive framework that encompasses the entire care process, from data collection to personalized treatment planning. This framework integrates data collection, storage, interoperability, analysis, benchmarking, assessment, value-based evaluation, and iterative improvement. It aligns the goals of sarcoma patients and healthcare providers. The framework outlines strategies for collecting real-world-time data, including measures and quality indicators from various sources. Thereby, the roadmap optimizes sarcoma care through data-driven approaches, collaboration, and iterative improvement (Figure 1).
2. Collection of Real-World-Time Data
Data collection in sarcoma care involves gathering real-world-time data from multiple sources to gain a comprehensive understanding of the longitudinal care journey. This process encompasses Clinical-Reported Outcome Measures (CROMS), which provide objective clinical indicators recorded by healthcare professionally, such as patients’ medical condition, treatment progress, and health outcomes. Patient-Reported Outcome Measures (PROMS) and Patient-Reported Experience (PREMS) capture subjective experiences, including quality of life, symptoms, functional abilities, and satisfaction with care. Holistically, it also involves DROMS (Diagnostic-Reported Outcome Measures), IROMS (Imaging-Reported Outcome Measures), FROMS (Functional-Reported Outcome Measures), SROMS (Safety-Reported Outcome Measures), and EROMS (Economic-Reported Outcome Measures).
Various sources are utilized to collect this diverse data, including electronic health records (EHR), surveys, interviews and focus groups. EHR provide comprehensive information on patients’ medical history, treatments, and outcomes. Surveys enable the gathering of additional patient-reported data, focusing on specific aspects of sarcoma care. Interviews and focus groups allow for in-depth qualitative data collection, providing with an opportunity to express their experiences and perspectives. By incorporating data from these different sources, the data collection process ensures a holistic representation of the sarcoma care journey. Such comprehensive evaluation approach allows healthcare professionals to assess both the medical outcomes and the patients’ experiences, needs, and satisfaction.
SSN has defined a set of some 500 parameters designed to assess the quality of sarcoma care. These include physician- as well as patient-based information and are collected from daily routine processes. Specifically, SSN published on the Sarcoma-specific instrument to longitudinally assess health-related outcomes of the routine care cycle.
3. Processing Data on an Interoperable Digital Platform (such as Sarconnector)
The use of an interoperable digital platform is crucial for securely storing and managing data in sarcoma care. This platform offers advantages in terms of data integration, accessibility, and analysis. It enables seamless integration of data from various sources, ensuring compatibility across different systems. Healthcare professionals can easily access and retrieve relevant data, promoting collaboration and evidence-based decision-making. The platform also supports effective data management, facilitating the processing of large and complex datasets. It provides tools for efficient data storage, organization, and retrieval, allowing healthcare professionals to navigate and analyze effectively (within a so-called data management ecosystem including data registry, data warehouse and data lake). Additionally, the platform serves as a foundation for subsequent analyses, incorporating advanced analytics techniques to uncover patterns and correlations within the data management ecosystem. Data security is prioritized through encryption, access controls, and adherence to privacy regulations. By leveraging an interoperable digital platform, healthcare professionals can efficiently access, manage, and analyze data, leading to improved decision-making and advancements in sarcoma care.
SSN has introduced the Sarconnector, an interoperable digital platform which allows harmonized data assessment from various sources to include all data dimensions.
4. Performing Automated Analysis on the Interoperable Digital Platform
Once sarcoma care data is securely stored on the interoperable digital platform, automated analysis becomes crucial. It utilizes tools and algorithms for statistical analysis, data mining, and machine learning. Statistical analysis uncovers patterns and trends, summarizing data characteristics and making predictions. Data mining techniques extract valuable insights from large data sets, revealing hidden patterns and anomalies. Machine learning algorithms learn from data to make predictions and optimize treatment decisions. Automated analysis empowers data-driven decisions, improving care strategies and patient outcomes. It uncovers associations between treatments and outcomes, identifies non-adherence factors, and enhances patient experiences. By continuously evaluating and refining practices, healthcare professionals deliver effective and patient-centered care. Therefore, automated analysis reveals insights, supports decision-making, and improves sarcoma care outcomes.
SSN’s Sarconnector is designed to synthesize meta-level data to integrate both descriptive, inferential, non-/parametric and Bayesian statistics, with its main focus on exploratory data analysis and its visualization.
5. Benchmarking against quality indicators
Benchmarking against quality indicators is essential for evaluating the effectiveness of sarcoma care. It involves comparing analyzed data against predefined standards specific to sarcoma care. These indicators provide measurable criteria for assessing healthcare performance and identifying areas of improvements.
Survival rates are crucial metrics that reflect treatment effectiveness and patient outcomes, recurrence rates indicate treatment success and the likelihood of cancer returning. Adherence to treatment guidelines evaluates the consistency of care delivery. Patient satisfaction scores capture subjective experiences and preferences, guiding improvements in care. Additional quality indicators include evidence-based practices, safety protocols, multidisciplinary care teams, follow-up care, and patient-centered principles. The choice depends on organizational goals and priorities.
Benchmarking allows healthcare professionals to assess their performance objectively and identify areas for improvement. It provides a quantitative assessment, highlighting specific aspects where standards may not be met. Furthermore, benchmarking facilitates learning from high-performing professionals and organizations. Analyzing their data reveals effective strategies and interventions, enabling others to enhance their care processes and outcomes. Benchmarking therefore is critically important for sarcoma care as it promotes continuous quality improvement. It empowers professionals to evaluate performance, implement interventions, and optimizes care delivery. By striving for excellence, sarcoma patients receive the highest quality care available.
SSN has introduced benchmarking by assessing a multilayer outcome to compare results from one’s own practices, processes, or outcomes to those of other organizations or practices in the same field, both nationally and internationally.
6. Assessment of Sarcoma Care
The assessment of sarcoma quality care involves evaluating various dimensions of care, including clinical outcomes, patient experiences, adherence to quality indicators, and relevant parameters. Clinical outcomes, such as survival rates and treatment responses, assess the effectiveness of interventions. Patient experiences, captured through PROMs and PREMs, provide insights into care satisfactions and patient centeredness. Adherence to quality indicators ensures evidence-based practices are followed. Safety measures, coordination of care, and communication are additional considerations. This assessment helps identify areas of improvement and strengths, guiding interventions and resource allocation. It promotes continuous learning and collaboration among healthcare professionals, facilitating knowledge exchange and improvement in sarcoma care. By prioritizing interventions based on assessment findings, healthcare professionals can enhance patient outcomes and experiences. The assessment contributes to overall knowledge and the development of best practices within the field. We expect from the assessment of sarcoma quality care to evaluate clinical outcomes, patient experiences, adherence to quality indicators, and relevant parameters. It guides improvement initiatives, fosters collaboration, and drives continuous enhancement in sarcoma care.
SSN introduced the quality indicators of sarcoma care together with an international advisory board of world-renowned sarcoma experts.
7. Value-based Healthcare Assessment
Value-based healthcare assessment evaluates sarcoma care by considering effectiveness, efficiency, and patient-centeredness. Metrics like cost-effectiveness, patient-reported value, and quality-adjusted life years (QALYs) are used to optimize value. Effectiveness measures outcomes achieved, such as survival rates and patient well-being, to identify best interventions. Efficiency assesses resource utilization in relation to outcomes, using cost-effectiveness analysis to guide resource allocation. Patient centeredness tailors care to individual needs, with patient-reported value capturing satisfaction and quality of life. QALYs measure quantity and quality of life gained through interventions, aiding decision-making. Other metrics like patient-reported outcomes and satisfaction scores provide additional insights. Value-based healthcare assessment aims to optimize value in sarcoma care, ensuring resources are allocated for maximum effectiveness, efficiency, and patient-centeredness. By integrating this assessment, healthcare professionals prioritize interventions that deliver the greatest value, leading to improved patient outcomes and experiences.
SSN has defined a value-based healthcare delivery model for sarcoma patients, and is able to correlate the clinical care efforts with financial expenses by use of the interoperable digital platform, the so-called Sarconnector.
8. Iterative Improvement Loop
The iterative improvements loop is crucial of enhancing sarcoma care based on assessment findings. It involves analyzing assessment results, identifying areas for improvement, and implementing targeted interventions to drive ongoing improvements in clinical outcomes, patient experience, and value delivered. After conducting the assessment, the healthcare team carefully reviews the findings and identifies opportunities for enhancement. Targeted interventions are then developed and implemented within the care process, such as changes to protocols, treatment pathways, patient education, coordination of care, or the adoption of new technologies. Feedback loops are established to monitor the impact of interventions, allowing healthcare professionals to assess effectiveness and make data-driven decisions, adjustments and refinements in sarcoma care, adapting to changing needs and best practices. By continuously refining the care process, healthcare professionals strive to provide the best possible care for sarcoma patients, enhancing outcomes and patient experience while optimizing value delivered.
SSN has established the Sarcoma Academy (www.sarcoma.academy), an international webinar forum for global exchange. This enables an up-to-date input from world-renowned experts of sarcoma care, and the potential to harmonize and share data on the global stage.
9. Predictive AI/ML Modelling
Predictive artificial intelligence (AI) and machine learning (ML) modeling techniques offer valuable insights and decision-making support. These techniques use real-world-time data to develop predictive models that forecast outcomes, identify high-risk patients, and guide treatment decisions.
Predictive AI/ML modeling involves training algorithms on historical data to identify patterns and make predictions or classifications. In sarcoma care, various techniques like decision trees, logistic regression, support vector machines, and deep learning algorithms can be employed.
-Forecasting future outcomes: by analyzing collected data, models can identify patterns contributing to disease progression, treatment response, or survival rates. This enables healthcare professionals to anticipate outcomes and plan interventions accordingly. For instance, predicting sarcoma recurrence allows monitoring high-risk patients closely and adjusting treatment plans.
-identifying high-risk patients: Models analyze data to pinpoint patients at greater risk of poor outcomes or complications. Healthcare professionals can prioritize resources and intervention for these patients, providing targeted care. Models can predict treatment-related side effects, allowing tailored supportive care.
-enhancing personalized treatment decisions: Analyzing patient-specific data like clinical characteristics and genetic profiles enables the identification of suitable treatment options. Tailoring interventions to individual patients improves effectiveness.
-uncovering hidden patterns: Insights on risk factors and treatment modalities associated with better outcomes inform care plans and resource allocation, thereby empowering healthcare professionals to optimize care delivery.
SSN’s Sarconnector includes currently a 5-year follow-up of patients, which paves the way for outcome studies. A current project for example identifies risk factors to develop Clavien-Dindo complications after sarcoma surgery.
10. Composing sarcoma Digital Twin
Over time, as more data is collected and analyzed, a digital twin of sarcoma care is created. This digital twin is a virtual replica of an individual patient that simulates the behavior of the care process. It incorporates the insights gained from predictive modeling and integrates patient-specific data, enabling the generation of personalized treatment plans. The digital twin serves as a powerful tool to optimize care, providing a platform for experimentation, scenario analysis, and continuous learning. It allows healthcare professionals to simulate the impact of different interventions, refine treatment strategies, and ultimately improve patient outcomes.
The digital twin allows physicians to simulate the impact of interventions, test various treatment options, and refine strategies to achieve optimal patient outcomes. It facilitates evidence-based decision-making and continuous learning, leading to improved care delivery. For patients, the digital twin offers personalized treatment based on individual characteristics and preferences. By incorporating patient-specific data such as treatment response, the digital twin tailors interventions to meet specific needs, enhancing precision and effectiveness of care. Patients thereby actively participate in decision-making, explore different treatment options, and understand potential outcomes. The digital twin empowers patients, improves treatment outcomes, and increases engagement in the care process.
Conclusions
The integration of real-world-time data, interoperable digital platforms, automated analysis, benchmarking, assessment, value-based healthcare evaluation, iterative improvement loops, predictive AI/ML modeling, and the creation of a sarcoma digital twin offer tremendous opportunities to advance sarcoma care. By embracing these steps, healthcare professionals can enhance the quality and effectiveness of care, optimize patient outcomes, and provide personalized treatment plans. Through continuous refinements and the application of data-driven methodologies, the future of sarcoma care holds great promise for improved patient experiences and ultimately better long-term outcomes.
SSN has established the basic requirements to realize precision care for sarcoma patients.
Further reading: