Simulation in medicine
Simulation can be defined as the reproduction of the essential features of a real-life situation to achieve education through experiential learning goals [1], [2]. The aim is to represent reality as closely as possible such that the trainee is convinced the simulated encounter replicates what would happen in a real-life situation [3]. This controlled environment promotes repeated practice in a setting that forgives failure, allowing the opportunity to learn from potential mistakes without causing harm to the patient [4], [5]. In surgery, the simulation also helps to enhance psychomotor skills, hand-eye coordination, and ambidextrous abilities, which is especially important for minimally invasive surgery (MIS) [6]. Repeatedly using surgical simulation tools reduces operative time, lowers complication rates, and improves patient outcomes [7].
Classification of surgical Simulators
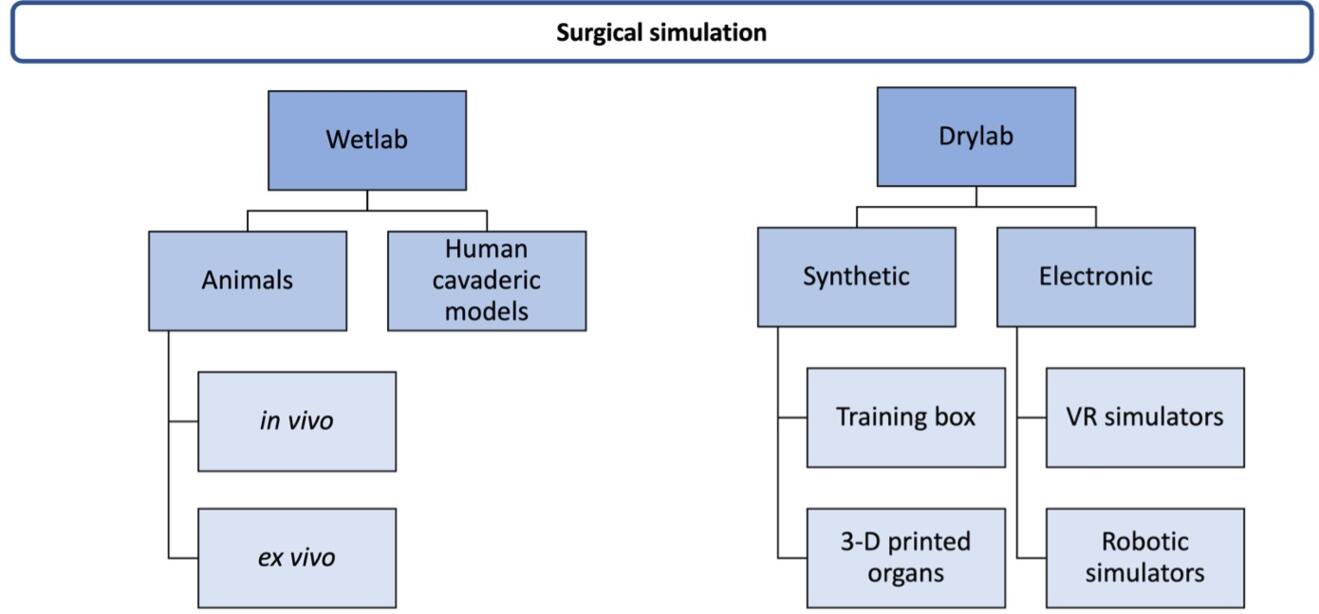
Surgical simulators can be divided into two main groups: wetlab and drylab (Fig. 1) [3]. Wetlab simulations consist of live animal and human cadaveric models with high-fidelity quality. However, many limitations regulate wetlab simulation, such as high costs, low accessibility, and ethical considerations [8]. Drylab simulators comprise electronic and synthetic bench models. Synthetic models are constructed from various materials and are conventionally used to teach basic procedures [9], [10]. In addition, box trainers familiarize trainees with two major aspects of laparoscopy: psychomotor control and visuospatial orientation [10].
Synthetic organs
The use of synthetic organs made of different materials can be tailored to provide realistic responses to incision, dissection, and suturing, thus enabling realistic tactile simulations in surgical training [11]. Developing and validating synthetic organs is especially important in urology, gynecology, and general surgery [12].
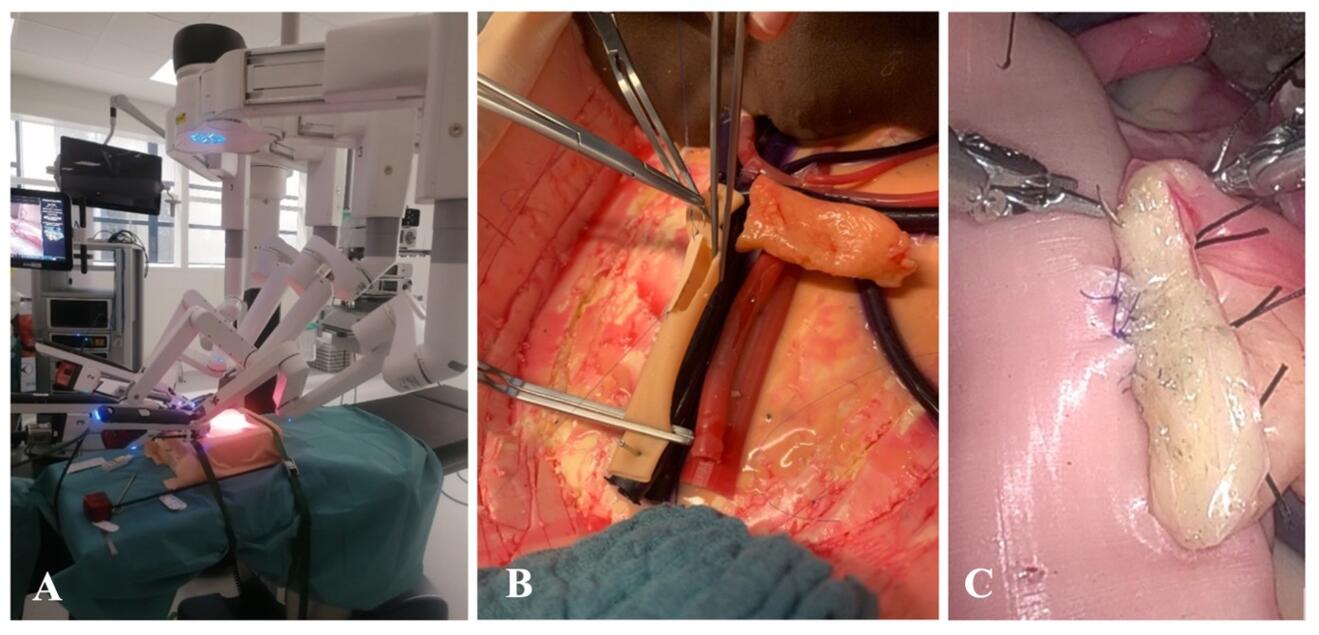
Thanks to material engineering, developing three-dimensional (3D) silicone organ models based on realistic patient anatomy is possible using different modeling and 3D printing technology [13]. Karadza et al. described a silicone BioTissue pancreas, bile duct, and small intestinal model to practice anastomotic suturing after pancreatoduodenectomy. The synthetic organ models showed high haptic realism and realistic suturing behavior and have successfully been used in professional courses and training (Fig. 2) [14].
Virtual Reality simulators
Virtual reality (VR) is a collection of technologies allowing people to interact efficiently with 3D computerized environments in real-time using their natural senses and skills [15]. The first models were introduced in the 1990s to broaden user interactivity and increase fidelity [16]. One of the first VR simulators was developed by surgeons collaborating with psychologists who designed a task analysis of laparoscopic cholecystectomy (LC) [3]. Most VR simulators are designed to teach laparoscopic and endoscopic procedures such as LC, appendectomy, inguinal hernia repair, and hysterectomy (Fig. 3) [17], [18]. A VR simulator allows the trainee to practice basic skills such as dissection, retraction, cutting, and suturing, as well as complete surgical procedures [19]. One of the most attractive features of the VR simulator is the ability to offer repetitive training with context, training programs, feedback, and instructions in a safe surgical setting for practicing outside of the OR [20], [21]. However, the main downside of the VR simulator reported in the current literature is the limited realism of haptic feedback and visual interaction with tissue, which somewhat restricts skill transfer to real-life surgery [22].
Immersive Virtual Reality
An extension of VR is immersive virtual reality (iVR), defined as an entirely virtual interactive simulation with a 3D environment projected onto a head-mounted display (HMD), allowing for 360° of visual immersion and real-time manipulation of virtual items [16]. This type of simulator creates a digital environment that replaces the user's real-world environment. The combination of iVR with machine learning (ML) and artificial intelligence (AI) is transforming virtual reality into an innovative tool not only for training reiterated technical schemes but also for providing personalized teaching and assessing skill acquisition [23].
Telestration and Augmented Reality
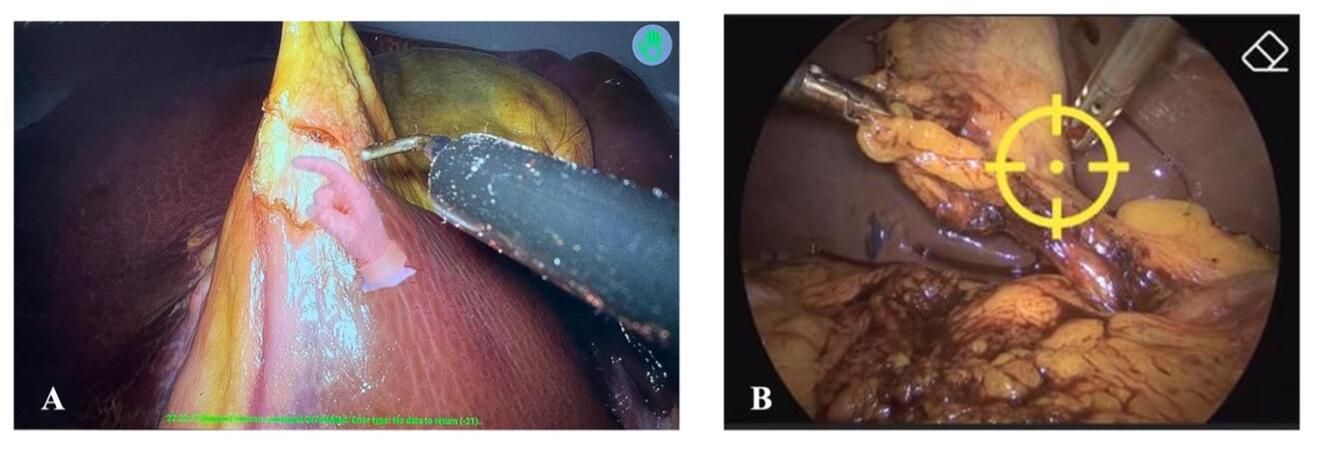
New technological advancement enabled the creation of telestration models with augmented reality (AR) to assist intraoperative expert guidance and training in MIS [24], [25]. One of the telestration models with AR, the iSurgeon, has shown a positive impact on MIS training in basic laparoscopic skills and LC compared to conventional verbal guidance (Fig. 4) [26], [27]. Furthermore, telestration models with AR, like iSurgeon, can provide effective MIS training and real-time intraoperative guidance during MIS procedures also remotely.
Robotic-assisted surgery and surgical simulators
Robotic-assisted surgery (RAS) has some advantages over laparoscopic surgery since it restores some of the visuospatial deficit through 3D stereoscopic visualization, eases instrument manipulation, and provides a stable platform and advantages for precise dissection and handling. Some RAS systems have eye-tracking functions and tremor filtering, enabling the surgeon to be more accurate [28]. RAS provides a perfect platform for the digitalization of surgery since it allows for both extraction of surgical data and the input of various kinds of information to support surgical performance. RAS potentially reduces workload and shortens the surgical learning curve compared to conventional laparoscopy [29]. Currently, RAS is widely used in various surgical disciplines, such as urology, gynecology, general, and cardiothoracic surgery [30]. Most RAS training focuses on developing the technical and cognitive skills required to operate at the surgical console, and some also provide full procedural simulations [31]. Some of the most widely used RASS simulators are SEP-Robot, RoSS, RobotiX Mentor dV-Trainer, and the da Vinci Skills Simulator [32].
Serious gaming
A novel concept in medical education is interactive learning through serious gaming. It is formally defined as an interactive computer application with a challenging goal, is fun to play, incorporates a scoring mechanism, and supplies the user with skills, knowledge, or attitudes helpful in reality [33], [34]. It can even be more efficacious than conventional methods of health professions education through increased engagement and immersion due to the game’s competitive element, fun, and interactivity [35], [36], [37]. However, one common barrier associated with game-based learning is the resources needed to develop and implement a successful activity [38].
A future approach in serious gaming could be implemented in the form of hybrid models that combine traditional teaching methods with a computer software component such as artificial intelligence. Thus, the surgical simulation could offer teaching programs providing valuable information for the trainees based on deep learning algorithms such as feedback, anatomy identification, and surgical outcome. Mascagni et al. described a deep learning model for laparoscopic cholecystectomy that can provide segmentation of the hepatocystic anatomy and predict Critical View of Safety (CVS) criteria achievement to avoid biliary and vascular injuries [39]. Such predictions in a controlled and simulated environment can potentially improve learning curves and patient safety.
Conclusions
The traditional Halstedian model, "see one, do one, teach one," is no longer acceptable since surgical simulations have become essential to contemporary surgical training and education and provide surgical training outside the operation room. This takes away part of the surgical learning curve from the patient side and thus improves care. The old paradigm now transforms into "see more, practice more, do more, teach more". The contemporary surgical training modalities provide a new shift in surgical training approach, enabling trainees in a patient-safe training environment to perfect their surgical skills.
- Tan SSY, Sarker SK. Simulation in surgery: a review. Scottish Medical Journal. 2011;56(2):104-109.
- Al-Elq AH. Simulation-based medical teaching and learning. J Family Community Med. 2010 Jan;17(1):35-40.
- Tan S, Sarker S. Simulation in Surgery: a review. Scottish Medical Journal. 2011, 104-109, 56(2).
- Badash I, Burrt K, Solorzano CA, Carey JN, Innovations in surgery simulation: a review of past, current and future techniques. Ann Transl Med 2016;4(23):453.
- Nickel F, Cizmic A, Chand M. Telestration and Augmented Reality in Minimally Invasive Surgery: An Invaluable Tool in the Age of COVID-19 for Remote Proctoring and Telementoring. JAMA Surg. 2022 Feb 1;157(2):169-170.
- Seymour NE, Gallagher AG, Roman SA. Virtual reality training improves operating room performance. Ann Surg. 2002;236(4):458–464.
- Zevin B, Aggarwal R, Grantcharov TP. Surgical simulation in 2013: why is it still not the standard in surgical training? J Am Coll Surg. 2014 Feb;218(2):294-301.
- S. K. Sarker; B. Patel. Simulation and surgical training. International Journal of Clinical Practice. 2007.61(12), 2120–2125.
- Berridge C. Jay S. Shekhar C. Current and future simulation in urological surgery training. Trends in Urology and Men´s Health. 2019 June.
- Nickel, F., Hendrie, J.D., Kowalewski, KF. et al. Sequential learning of psychomotor and visuospatial skills for laparoscopic suturing and knot tying—a randomized controlled trial “The Shoebox Study”. Langenbecks Arch Surg 401, 893–901 (2016).
- Kilic D, Ustbas B, Budak EP, Eyisoylu H, Yilmaz C, Eldem B, Akbulut O. Silicone-based composites as surgical breast models for oncoplasty training. Procedia Eng. 2016;159:104–107. doi: 10.1016/j.proeng.2016.08.131.
- Sankaranarayanan G, Parker L, De S, Kapadia M, Fichera A. Simulation for Colorectal Surgery. J Laparoendosc Adv Surg Tech A. 2021 May;31(5):566-569.
- Pugliese L, Marconi S, Negrello E, Mauri V, Peri A, Gallo V, Auricchio F, Pietrabissa A. The clinical use of 3D printing in surgery. Updates Surg. 2018 Sep;70(3):381-388.
- Karadza E, Haney CM, Limen EF, Müller PC, et al. Development of biotissue training models for anastomotic suturing in pancreatic surgery. HPB (Oxford). 2023 Feb 9:S1365-182X (23) 00041-2.
- McCloy R, Stone R. Science, medicine, and the future. Virtual reality in surgery. BMJ. 2001 Oct 20;323(7318):912-5.
- Mao RQ, Lan L, Kay J, Lohre R, Ayeni OR, Goel DP, Sa D. Immersive Virtual Reality for Surgical Training: A Systematic Review. J Surg Res. 2021 Dec;268:40-58.
- Beyer-Berjot L, Aggarwal R. Toward technology-supported surgical training: the potential of virtual simulators in laparoscopic surgery. Scand J Surg. 2013;102(4):221-6.
- Nickel F, Hendrie JD, Stock C, Salama M, Preukschas AA, Senft JD, Kowalewski KF, Wagner M, Kenngott HG, Linke GR, Fischer L, Müller-Stich BP. Direct Observation versus Endoscopic Video Recording-Based Rating with the Objective Structured Assessment of Technical Skills for Training of Laparoscopic Cholecystectomy. Eur Surg Res. 2016;57(1-2):1-9.
- Clarke, E. Virtual reality simulation—the future of orthopaedic training? A systematic review and narrative analysis. 2021; Adv Simul 6, 2.
- Kenngott HG, Wagner M, Nickel F, Wekerle AL, Preukschas A, Apitz M, Schulte T, Rempel R, Mietkowski P, Wagner F, Termer A, Müller-Stich BP. Computer-assisted abdominal surgery: new technologies. Langenbecks Arch Surg. 2015 Apr;400(3):273-81.
- Nickel F, Brzoska JA, Gondan M, Rangnick HM, Chu J, Kenngott HG, Linke GR, Kadmon M, Fischer L, Müller-Stich BP. Virtual reality training versus blended learning of laparoscopic cholecystectomy: a randomized controlled trial with laparoscopic novices. Medicine (Baltimore). 2015 May;94(20):e764.
- Nickel F, Bintintan VV, Gehrig T, Kenngott HG, Fischer L, Gutt CN, Müller-Stich BP. Virtual reality does not meet expectations in a pilot study on multimodal laparoscopic surgery training. World J Surg. 2013 May;37(5):965-73.
- Veneziano D, Cacciamani G, Rivas JG, Marino N, Somani BK. VR and machine learning: novel pathways in surgical hands-on training. Curr Opin Urol. 2020 Nov;30(6):817-822.
- Jarc AM, Shah SH, Adebar T, Hwang E, Aron M, Gill IS, Hung AJ. Beyond 2D telestration: an evaluation of novel proctoring tools for robot-assisted minimally invasive surgery. J Robot Surg. 2016 Jun;10(2):103-9.
- Kowalewski KF, Hendrie JD, Schmidt MW, Garrow CR, Bruckner T, Proctor T, Paul S, Adigüzel D, Bodenstedt S, Erben A, Kenngott H, Erben Y, Speidel S, Müller-Stich BP, Nickel F. Development and validation of a sensor- and expert model-based training system for laparoscopic surgery: the iSurgeon. Surg Endosc. 2017 May;31(5):2155-2165.
- Wild C, Lang F, Gerhäuser AS, Schmidt MW, Kowalewski KF, Petersen J, Kenngott HG, Müller-Stich BP, Nickel F. Telestration with augmented reality for visual presentation of intraoperative target structures in minimally invasive surgery: a randomized controlled study. Surg Endosc. 2022 Oct;36(10):7453-7461.
- Felinska EA, Fuchs TE, Kogkas A, Chen ZW, Otto B, Kowalewski KF, Petersen J, Müller-Stich BP, Mylonas G, Nickel F. Telestration with augmented reality improves surgical performance through gaze guidance. Surg Endosc. 2023 Jan 6.
- Rogula T, Myszka A, Vongsurbchart T, et. Al. Robotic surgery training, simulation, and data collection. Simulations in Medicine, Computer aided diagnostics and therapy. 2020, (pp.150-167) Chapter 11. De Gruyter.
- Willuth E, Hardon SF, Lang F, Haney CM, Felinska EA, Kowalewski KF, Müller-Stich BP, Horeman T, Nickel F. Robotic-assisted cholecystectomy is superior to laparoscopic cholecystectomy in the initial training for surgical novices in an ex vivo porcine model: a randomized crossover study. Surg Endosc. 2022 Feb;36(2):1064-1079.
- Maeso S, Reza M, Mayol JA et al. Efficacy of the da Vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis. Ann Surg 2010; 252: 254–62.
- Wang RS, Ambani SN. Robotic Surgery Training: Current Trends and Future Directions. Urol Clin North Am. 2021 Feb;48(1):137-146.
- Liu M, Curet M. A review of training research and virtual reality simulators for the da Vinci surgical system. Teach Learn Med 2015;27:12-26.
- Bergeron BP. Developing Serious Games. Charles River Media: Hingham, Mass 2006.
- Graafland M, Schraagen JM, Schijven MP. Systematic review of serious games for medical education and surgical skills training. Br J Surg. 2012 Oct;99(10):1322-30.
- Haoran G, Bazakidi E, Zary N. Serious Games in Health Professions Education: Review of Trends and Learning Efficacy. Yearb Med Inform. 2019 Aug;28(1):240-248.
- Wang R, DeMaria S Jr, Goldberg A, Katz D. A Systematic Review of Serious Games in Training Health Care Professionals. Simul Healthc. 2016 Feb;11(1):41-51.
- Xu M, Luo Y, Zhang Y, Xia R, Qian H, Zou X. Game-based learning in medical education. Front Public Health. 2023 Mar 3;11:1113682.
- Oestreich JH, Guy JW. Game-Based Learning in Pharmacy Education. Pharmacy (Basel). 2022 Jan 6;10(1):11.
- Mascagni P, Vardazaryan A, Alapatt D, et. Al. Artificial Intelligence for Surgical Safety: Automatic Assessment of the Critical View of Safety in Laparoscopic Cholecystectomy Using Deep Learning. Ann Surg. 2022 May 1;275(5):955-961.