Case description:
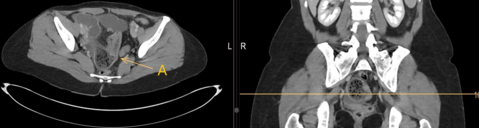
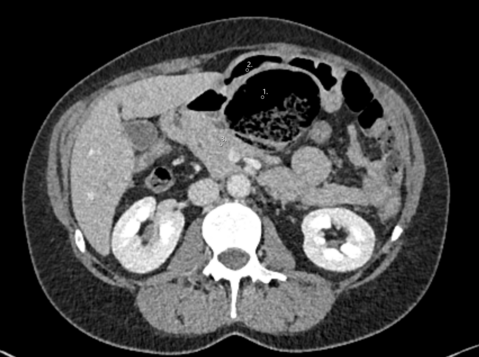
A 76-year-old patient with cerebral palsy who has experienced sporadic intermittent painless scleral and cutaneous jaundice is referred to surgery consultation for evaluation of cholecystectomy for cholecystolithiasis. As a young man the military service was interrupted because of jaundice. Injection drug use, alcohol drinking, or infectious infections are not known to have occurred. There are no other secondary diagnoses relevant to this case. The clinical examination is unremarkable. Laboratory values show an isolated bilirubinemia (total bilirubin 91 µmol/l, direct bilirubin 33 µmol/l). The rest of the hematologic findings are within normal limits. A prior abdominal ultrasound shows cholecystolithiasis with a hydroptic gallbladder. Computertomography reveals no pancreatic mass. An MRCP (magnetic resonance cholangiopancreatography) could not be performed due to cerebral palsy. Therefore, another EUS (Endoscopic ultrasound) was performed immediately before starting with the laparoscopy to have a bimodal exclusion of pancreatic tumors. No familiarity for pancreatic tumors.
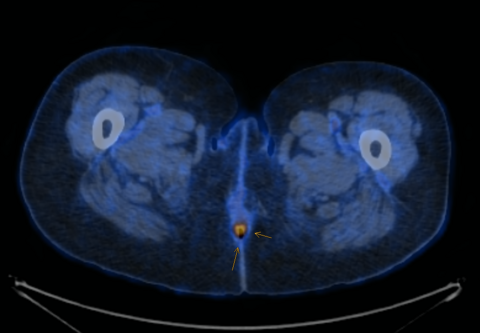
Intraoperatively a smooth liver with normal consistency and morphology but with a grossly black colour was revealed (see figure 1 and 2).
What is the possible diagnosis?
- Hemochromatosis
- Dubin-Johnson-Syndrom
- Biliary cirrhosis
- Rotor Syndrom
- Crigler-Najjar Syndrome
Case solution:
The correct answer is: Dubin-Johnson-Syndrom (DJS)
The typical picture of a black liver in Dubin-Johnson-Syndrome is seen in the laparoscopy images. DJS is a rare autosomal recessive liver disease presenting with mixed conjugated and unconjugated isolated bilirubinemia due to defective bilirubin excretion caused by a defect of MRP2 gene[1] [2] (see table 1). Liver biopsies show extensive, partially pericenter accentuated deposition of dark brownish granular pigment and confirm the suspected diagnosis histologically [3]. Further therapeutic measures do not need to be initiated, and there is no increased risk of fibrosis or cirrhosis3 [4].
Hereditary hyperbilirubinemias
| Gilbert-Meulengracht | Crigler-Najjar | Dubin-Johnson-Syndrome | Rotor Syndrome |
Mechanism | Defective conjugation activity | Defective glucuronidation | Biliary transport deficiency | Defective hepatic storage of conjugated bilirubin |
Level and type of Bilirubinemia | Fluctuating, unconjugated | Permanent, unconjugated | Fluctuating, unconjugated = conjugated | Fluctuating |
- Morais MB, Machado MV. Benign inheritable disorders of bilirubin metabolism manifested by conjugated hyperbilirubinemia-A narrative review. United European Gastroenterol J. 2022 Sep;10(7):745-753. doi: 10.1002/ueg2.12279. Epub 2022 Jul 20. PMID: 35860851; PMCID: PMC9486497.
- Keitel V, Nies AT, Brom M, Hummel-Eisenbeiss J, Spring H, Keppler D. A common Dubin-Johnson syndrome mutation impairs protein maturation and transport activity of MRP2 (ABCC2). Am J Physiol Gastrointest Liver Physiol. 2003 Jan;284(1):G165-74. doi: 10.1152/ajpgi.00362.2002. Epub 2002 Oct 2. PMID: 12388192.
- Strassburg CP. Hyperbilirubinemia syndromes (Gilbert-Meulengracht, Crigler-Najjar, Dubin-Johnson, and Rotor syndrome). Best Pract Res Clin Gastroenterol. 2010 Oct;24(5):555-71. doi: 10.1016/j.bpg.2010.07.007. PMID: 20955959.
- Memon N, Weinberger BI, Hegyi T, Aleksunes LM. Inherited disorders of bilirubin clearance. Pediatr Res. 2016 Mar;79(3):378-86. doi: 10.1038/pr.2015.247. Epub 2015 Nov 23. PMID: 26595536; PMCID: PMC4821713.