Case description:
A 52-year-old man presented to the emergency department with acute abdominal pain and bloody tinged output through the stoma. He has a medical history of multiple sclerosis, peripheral arterial disease and suspected yet undetermined and untreated inflammatory bowel disease. Due to a complicated course after laparoscopic sleeve resection and ischemia of the ascending colon, the patient had previously undergone a right hemicolectomy with terminal ileostomy.
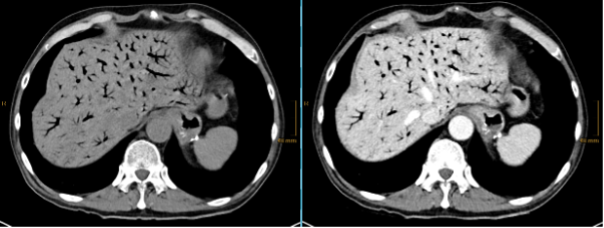
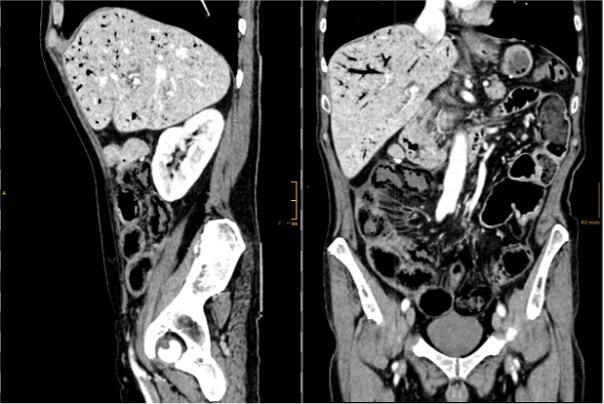
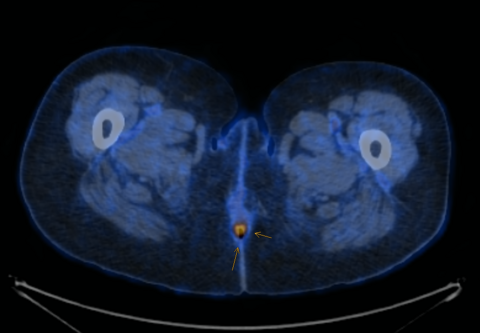
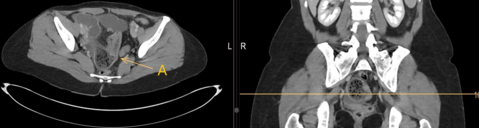
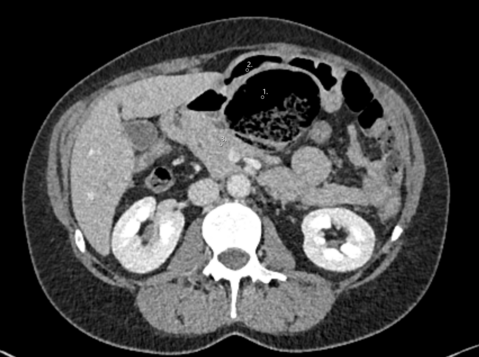
On presentation, he was stable with normal vital signs. Clinical examination revealed a diffusely tender abdomen, but no signs of peritonitis. Laboratory analysis showed WBC count of 26.8 G/l, CRP 99 mg/l, lactate 1.5 mmol/l. Computed tomography of the abdomen was performed and showed the findings below:
What is the appropriate next step in the management of this patient
· Surveillance on intensive care unit
· Emergency surgery
· No action needed as aerobilia can be managed conservatively
· Endoscopy
The correct answer is: B
CT scan showed an extensive aeroportia. Hepatic portal venous gas is mostly a serious condition and can indicate poor prognosis. Possible etiologies of pneumatosis intestinalis (PI) and portal venous gas (PVG) include intestinal ischemia caused by embolism, thrombosis, non-occlusive mesenteric ischemia, infections, recent abdominal trauma or inflammatory bowel diseases(1). Further, oncological therapies or immunosuppressive drugs have been reported to be the cause of pneumatosis intestinalis(2).
Management depends on general condition of the patient and the clinical examination.
In our case, an emergency laparotomy was performed because of a high suspicion of intestinal ischemia, especially considering the previous medical history. To our surprise and relief, no intraoperative evidence of intestinal ischemia was found. Postoperatively, detailed workup by gastroenterologists and rheumatologists did not reveal any conclusive findings to explain the cause of extensive PI and PVG. There was also no evidence of infection, drug abuse or medication that could explain the finding. In the interdisciplinary case discussion at the autoimmune board, chronic inflammatory bowel disease was ultimately seen as the most likely cause.
Postoperative recovery was unremarkable and a postoperative follow-up abdominal CT scan showed no remaining signs of PI and PVG.In case of PI and PVG, there is the option of close clinical follow-up as an alternative to emergency surgery, depending on the degree of clinical suspicion of ischemia. However, in the presence of peritonitis, clinically unstable patients or a high pre-test probability of intestinal ischemia, abdominal exploration is clearly recommended(3).
Radiologically, it is also important to distinguish an aeorportia from an aerobilia, as this is a completely separate clinical condition with distinct differential diagnoses and treatment algorithms(4).
- Latif E, Ahmed K, Zarour A. Extensive Aeroportia, Operate or Not to Operate? A Report of a Challenging Case. Cureus. 2021;13(2):e13295.
- Gazzaniga G, Villa F, Tosi F, Pizzutilo EG, Colla S, D'Onghia S, et al. Pneumatosis Intestinalis Induced by Anticancer Treatment: A Systematic Review. Cancers (Basel). 2022;14(7).
- Gonda M, Osuga T, Ikura Y, Hasegawa K, Kawasaki K, Nakashima T. Optimal treatment strategies for hepatic portal venous gas: A retrospective assessment. World J Gastroenterol. 2020;26(14):1628-37.
- Sherman SC, Tran H. Pneumobilia: benign or life-threatening. J Emerg Med. 2006;30(2):147-53.