The differential diagnosis of perianal swelling includes hemorrhoids, skin tags, and other benign conditions. However, not all perianal swellings turn out to be the most obvious or common diagnosis.
Case description
A 79-year-old female was referred to our unit for the evaluation of a persistent perianal swelling. The lesion had been present for several months, with recent increase in size. The patient reported a sensation of prolapse, perianal pruritus, occasional spotting of blood on toilet paper, and initial pain, which has since subsided. Bowel movements were regular in frequency and consistency. A recent colonoscopy was without abnormalities. Her medical history includes type 2 diabetes mellitus, coronary artery disease and arterial hypertension. She takes low-dose aspirin as her only regular medication.
Clinical examination revealed a firm, dark-livid, 1.5 cm perianal nodule at the 8 o’clock position. No additional anal abnormalities or skin tags were observed, and digital rectal examination and anoscopy were unremarkable. The referring clinic had previously performed an incision of the lesion; however, no thrombus could be evacuated.
Which is the most likely diagnosis?
A) Anal skin tag
B) Anal carcinoma
C) Thrombosed external hemorrhoids
D) Condyloma accuminatum
E) Malignant melanoma
Case solution
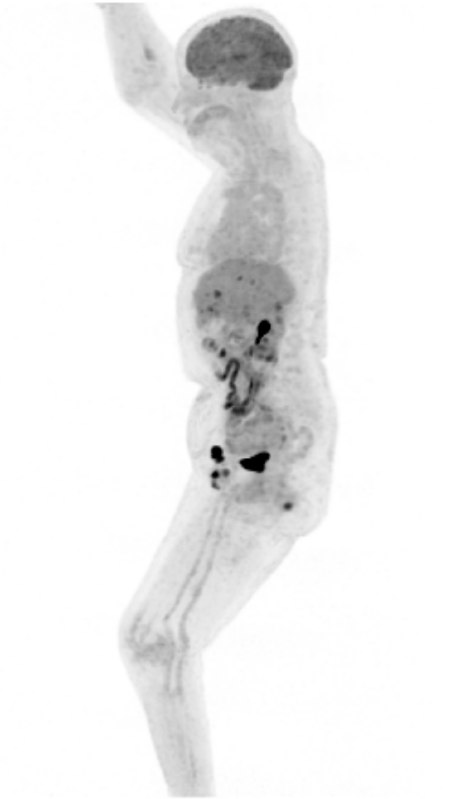
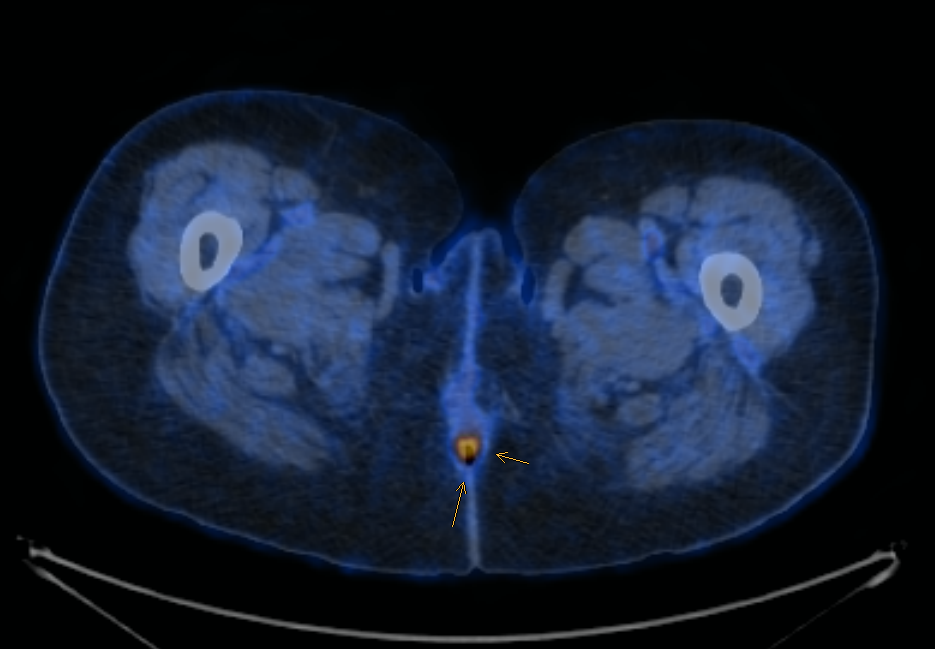
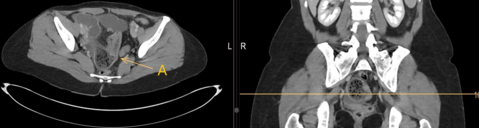
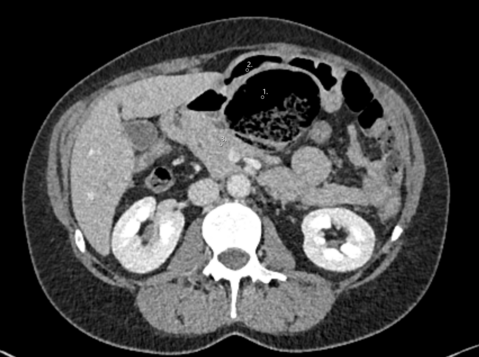
Biopsy revealed a malignant mucosal melanoma. Staging with PET-CT demonstrated additional metastatic inguinal lymph nodes (see Image 2). The case was discussed at our multidisciplinary tumor board in collaboration with dermatology. A local excision followed by adjuvant immunotherapy with Ipilimumab and Nivolumab was recommended. The colorectal surgery team performed a local excision, achieving complete (R0) resection of the tumor.
Mucosal melanoma is rare, accounting for <1% of all malignant melanomas (1). It predominantly affects older individuals, with a median age at diagnosis of 70 years (2). Prognosis is significantly worse than for cutaneous melanoma: the 5-year survival rate for mucosal melanoma is approximately 25%, and for anorectal mucosal melanoma, it drops to 20% (3). Whenever feasible, complete (R0) resection should be performed by a team of experienced colorectal surgeons and a surgical resection should be done in the least radical manner that allows for clear margins (R0) (4, 5).
- Olla D, Neumeister MW. Mucosal Melanoma. Clin Plast Surg. 2021;48(4):707-11.
- Yde SS, Sjoegren P, Heje M, Stolle LB. Mucosal Melanoma: a Literature Review. Curr Oncol Rep. 2018;20(3):28.
- Lerner BA, Stewart LA, Horowitz DP, Carvajal RD. Mucosal Melanoma: New Insights and Therapeutic Options for a Unique and Aggressive Disease. Oncology (Williston Park). 2017;31(11):e23-e32.
- Smith HG, Bagwan I, Board RE, Capper S, Coupland SE, Glen J, et al. Ano-uro-genital mucosal melanoma UK national guidelines. Eur J Cancer. 2020;135:22-30.
- Garbe C, Amaral T, Peris K, Hauschild A, Arenberger P, Basset-Seguin N, et al. European consensus-based interdisciplinary guideline for melanoma. Part 2: Treatment - Update 2024. Eur J Cancer. 2025;215:115153.