The aim of the guideline is to create a basis for interdisciplinary collaboration in the care of severely injured patients. The revision of the latest version of the document (released in 20162) aims to implement the most recent evidence-based recommendations. S3 guidelines are subject to the specifications of the German Association of Scientific Medical Societies (AWMF) and are considered the highest-quality version of the AWMF guidelines. In contrast to S1 (an opinion of a group of experts) and S2 (a formal consensus group: guidelines are developed from conclusions in the scientific literature that have been formally evaluated and debated in an established formal consensus process), a systemic development-process is required for S3 guidelines.
The German Trauma Surgery (DGU) has the lead in this project. The formulated recommendations relate to medical care structures in Germany. However, the new guidelines are also of great importance for Switzerland, as the organization and patient populations in Switzerland are very similar3.
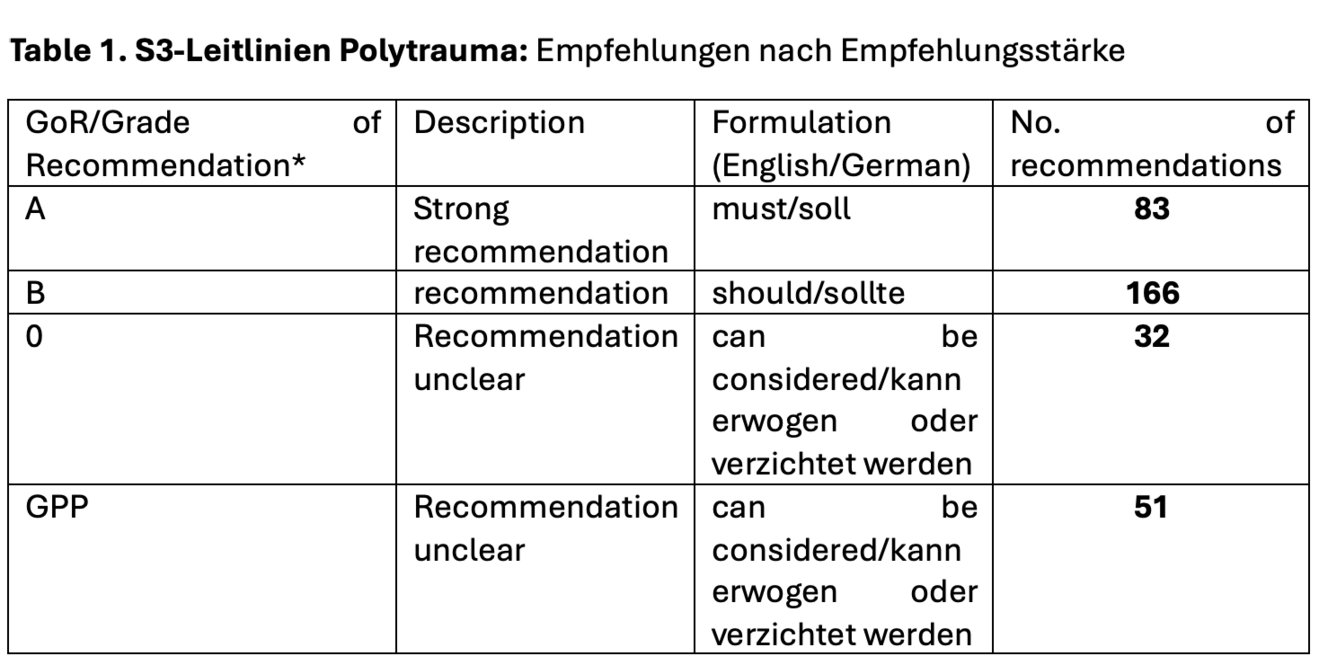
The revision of the previous S3 guideline started in March 2020. A total of 26 medical societies and professional associations were involved. All working groups presented their findings at five different consensus conferences, and a standardized voting process ultimately resulted in 332 consensus-based recommendations. For guideline recommendations to be effective, they should be clear and specific. The grading of the recommendations can be derived from the quality of the available literature. Table 1 provides an overview of the number of recommendations in the new S3 guideline by strength of recommendation, as well as their description and wording requirements.
*GoR: Grade of Recommendation; GPP: Good (clinical) Practice Point/Expert consensus, no suitable literature is available.
The entire trauma chain - from the accident site to surgical treatment - is covered in the guideline. The guideline is organized into three different subject areas:
i. prehospital phase
ii. shock room/emergency department phase
ii. first operative phase/primary operative management
The new S3 guideline contains a total of 40 chapters, including 2 completely new chapters, >14,000 references, 69 new and 70 modified key recommendations. For the revision of the individual chapters, one or more literature searches were carried out in various databases.
Each subject area is divided into several chapters. The prehospital phase contains 10 chapters, five of which have been revised using a structured literature review, and two completely new chapters ('Stop the bleeding' and 'Analgesia'). The prehospital phase has 98 recommendations, 24 of which are GoR A. As an example of a new GoR A recommendation in the new chapter 'Stop the bleeding', the following was adopted with a consensus strength of 96 %: 'For bleeding stab wounds in which the foreign body has already been removed and which are at least 3 cm in length, direct wound tamponade with chitosan should be applied'.
In addition, another interesting new GoR A recommendation was adopted with a consensus of 100 %: 'In trauma patients in whom venous access is unsuccessful, an intraosseous needle should be placed for infusion and drug therapy'.
The 'shock room phase' section consists of a total of 17 chapters, 10 of which have been revised. There are 139 recommendations, 36 of which are GoR A recommendations. Interestingly, the shock room activation criteria have been changed in order to counteract overloading of shock rooms and to reduce undertriage. Newly, pathological findings with clearly defined, measurable thresholds should lead to activation of the shock room team. The following criteria have been defined:
A/B-criteria: respiratory distress (SpO2<90) or need for airway protection, AF <10/>29.
C-criteria: systolic blood pressure <90 mmHg, heart rate > 120/min, shock index >0.9, positive eFAST
D-criteria: GCS ≤ 12
E-criteria: body core temperature < 35.0oC
These criteria are adopted as GoR A recommendation with a consensus strength of 94 %. In addition, certain injuries such as unstable pelvic or thoracic wall injuries or pre-hospital interventions remain activation criteria for the shock room team. There are also new recommendations on coagulation management. For example, coagulation diagnostics and therapy should be controlled by viscoelastic testing (GoR A recommendation).
Regarding the 'first operative phase', 6 out of 13 chapters were revised. A total of 95 recommendations are provided (GoR A:16, GoR B: 51, GoR 0:18, GPP:10).
The 'lower extremities'-chapter has been altered markedly. In the newest version of this chapter, the systemic status of patients with lower extremity injured is taken into account. These two new GoR B recommendations with a consensus strength of 100 pct. have been included in the guideline: i. If possible, isolated and multiple lower-extremity fractures should be managed with primary definitive fixation in patients whose condition is stable. And ii., If possible, patients whose condition is not considered stable should be managed with primary temporary fixation.
Of note, it is also interesting that some recommendations have remained unchanged, despite current global trends in the management of trauma patients. For example, the recommendations on immobilization of the cervical spine in the preclinical phase have not been adapted. Maybe the recommendations on this issue will change in the new version of the guideline, which is planned for the end of 2027.
We recommend that all those involved in caring for polytraumatized patients read the full 483 pages or the exciting abridged version (also available free of charge).
1 https://register.awmf.org/de/leitlinien/detail/187-023
2 Polytrauma Guideline Update Group. Level 3 guideline on the treatment of patients with severe/multiple injuries. Eur J Trauma Emerg Surg 44 (Suppl 1), 3–271 (2018). https://doi.org/10.1007/s00068-018-0922-y
3 Jensen KO, Teuben MPJ, Lefering R, Halvachizadeh S, Mica L, Simmen HP, Pfeifer R, Pape HC, Sprengel K; TraumaRegister DGU. Pre-hospital trauma care in Switzerland and Germany: do they speak the same language? Eur J Trauma Emerg Surg. 2021 Aug;47(4):1273-1280. doi: 10.1007/s00068-020-01306-3.