Complications after surgery – still a thing?
Despite significant advances in surgical techniques, anaesthesia, analgesia, and perioperative care, complication rates following major surgery remain unacceptably high—affecting 10–50% of patients and including life‑threatening events (1-3). It is increasingly clear that the success of an operation extends beyond the procedure itself to include the patient’s ability to regain physical activity and psychological well‑being. Optimal outcomes therefore depend not only on surgical expertise but also on structured strategies that support recovery and resilience.
Long term impact of low preoperative fitness
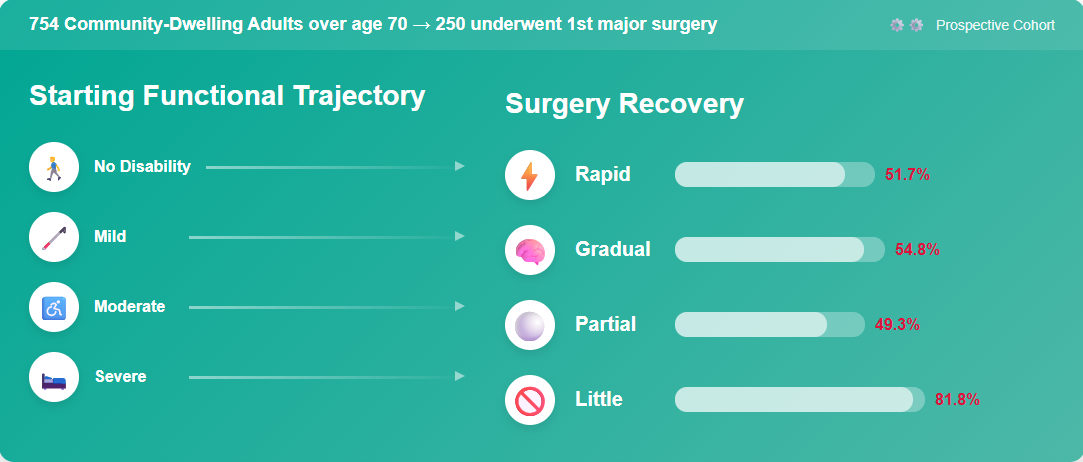
Evidence indicates that poor physical fitness is associated with adverse outcomes following surgery (4). At three months after major elective surgery, up to half of patients still experience significant disability (5). Similarly, when functional capacity is measured after abdominal surgery, only 30% of patients have returned to baseline by eight weeks and 50% by six months postoperatively (5, 6). Functional prognosis in the year after major surgery is therefore highly dependent on premorbid function (7).
Before there was the Enhanced Recovery After Surgery Program…
Perioperative medicine seeks to deliver a personalized, patient‑centered, multidisciplinary care pathway—from preoperative assessment through postoperative recovery—designed to minimize risk, reduce complications, and promote full restoration of health (8). Since the introduction of the enhanced recovery after surgery program (ERAS) in the 1990’s led by Hendrik Khelet and colleagues, multiple studies and meta-analyses have confirmed its positive impact. Compared to traditional care, enhanced recovery after surgery programs were associated with significantly decreased primary hospital stay, total hospital stay, total complications, as well as hospital acquired infections, non–procedure-specific complications and improved patient experience (9-12).
…then came Multimodal Prehabilitation
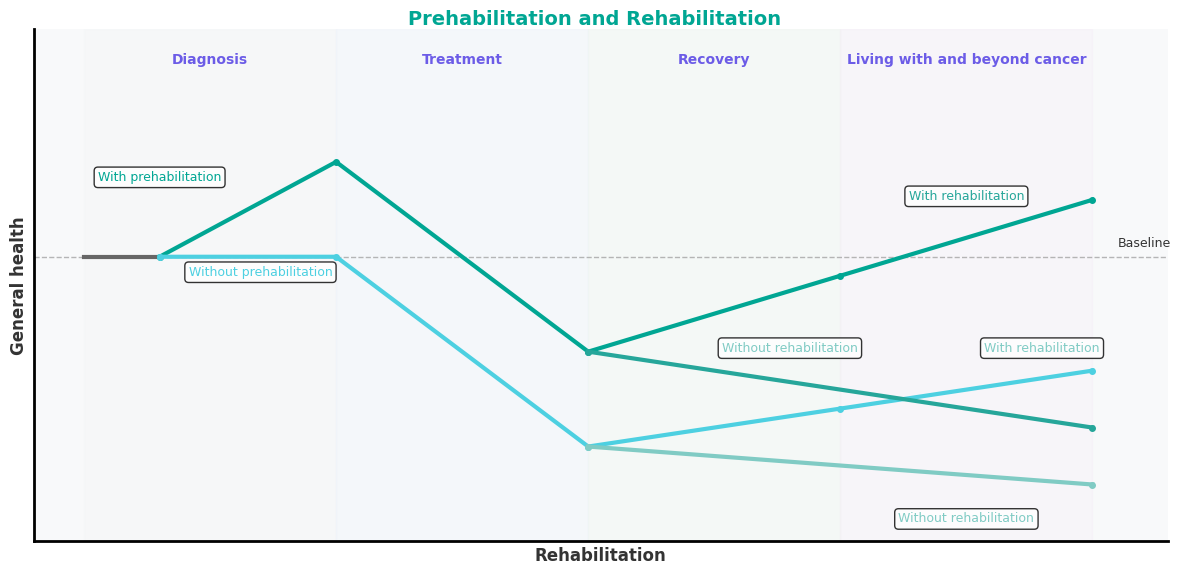
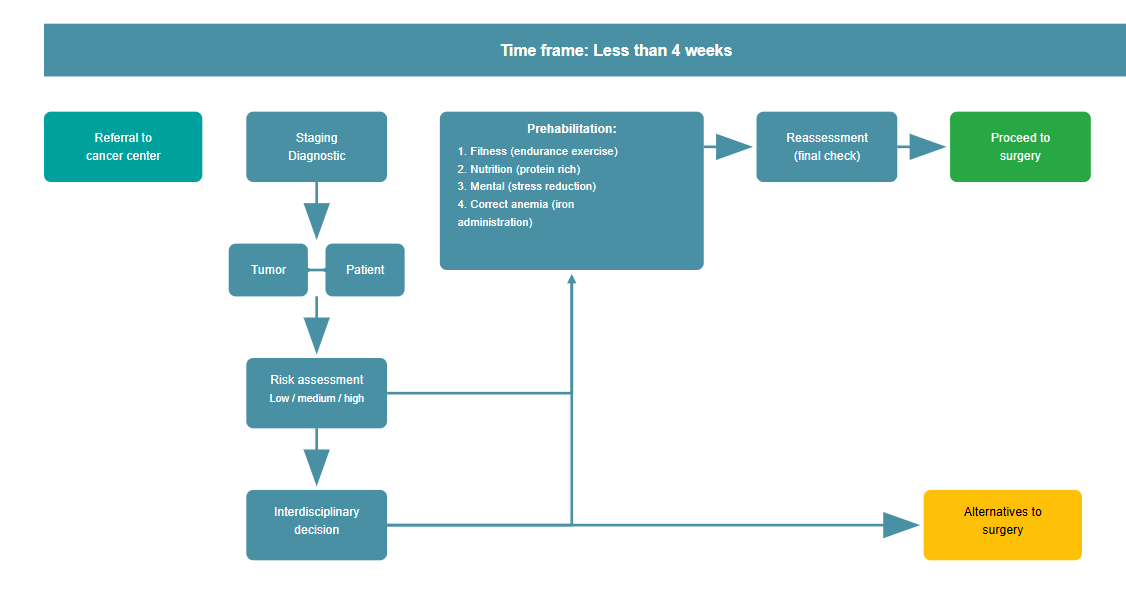
The term prehabilitation emerges in medical sports literature 40 years ago in the context of rehabilitation following an injury and preventing unnecessary atrophy (13) or to avert further injuries (14). Prehabilitation was also a program to prepare soldiers for battle of the second World War with proper food, lodging, hygiene, and controlled physical training and education (15). In current medical literature, prehabilitation is described as a program of enhancing functional capacity of an individual to enable him or her to better withstand an upcoming stressful event (16). By improving the individual’s functional capacity, the patient would maintain a higher level of functioning, thus resulting in a facilitated and accelerated recovery. Functional capacity is the term used to reflect the ability to perform activities of daily living and is determined by the integrity of the pulmonary, cardiovascular, and musculoskeletal systems. The preoperative period is understandably the opportune time to promote prehabilitation, and to act on physical unfitness, malnutrition, and anxiety while patients are waiting for surgery. Pre-operative modification of the high-risk patient includes both lifestyle changes and medical optimisation of comorbidities (17, 18). Several original studies and systematic reviews show a positive impact of prehabilitation on physical function and quality of life (19-22). Since it has been proven that the number and severity of complications are closely related to the preoperative function of the individual, there has been increasing interest in targeting these issues with a multimodal intervention program (23). From a physiological point of view, it seems feasible to achieve clinically relevant effects during a period of 2-4 weeks. However, this can only be achieved with targeted interventions including exercise, nutritional intervention, treatment of anaemia, smoking cessation and psychological support (24). An additional benefit can be expected from the empowerment of patients, who may then play a more active role in coping with their disease by preparing themselves for their upcoming surgery. An optimal recovery after surgery will also increase the potential of patients to withstand additional therapies such as chemotherapy, metastatic disease resection and more (25).
Current evidence – not great (yet)
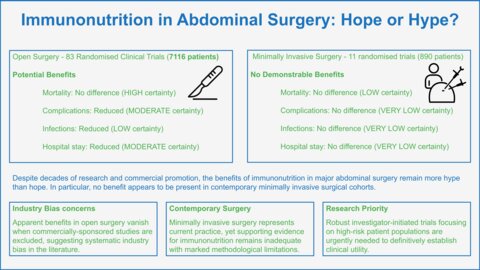
It began with the establishment of unimodal prehabilitation in the first years of its introduction; multimodal prehabilitation (education, exercise incl. inspiratory muscle training, nutrition, psychologic support) is now the preferred form of prehabilitation when available by leading experts today (18, 26). Many of the early studies investigating the effect of prehabilitation were only unimodal in nature (mostly exercise), had inadequate reporting, did not properly select patients at risk or had other shortcomings (27). As a consequence, in a recent umbrella review of 55 systematic reviews on prehabilitation, only 15 individual reviews could be pooled for meta-analyses to measure the overall certainty of effect as a result of heterogeneity. Despite this limitation, prehabilitation was found to improve functional recovery after oncological surgeries with moderate certainty, while the certainty of the evidence for non-oncological surgeries was rated as low or critically low (28).
It is plausible to hypothesise that patients at greater risk for postoperative complications, such as the frail elderly (a fast growing patient population), are more likely to benefit from prehabilitation (29). Another population most probably to benefit from such a program are cancer patients with decreased functional health after cancer treatment (30). Cancer prehabilitation offers an opportunity for the patient to improve functional status while awaiting treatment. This is likewise a patient group expected to grow in the future (31).
Preoperative Risk factors – the big three
Exercise capacity. Low physiological reserve respectively reduced aerobic fitness measured by cardiopulmonary exercise testing (CPET) is associated with increased postoperative morbidity and mortality (32). Further, ventilatory inefficiency, namely an increase in ventilation relative to the elimination of carbon dioxide, commonly quantified as VE/VCO2 slope, has also been identified as a prognostic marker for postoperative morbidity and mortality (33-37).
Malnutrition and surgical stress. Prospective cohort studies have shown that diagnose-related malnutrition significantly worsens clinical outcome in the perioperative phase, including increased odds of complications, as much risk of mortality, readmissions, prolonged length of hospital stay (LOS) and increased healthcare costs (38-42). The surgical trauma itself leads to metabolic reaction characterised by hormonal, haematological, metabolic and immunological alterations, defined as surgical stress response (42-44). The release of stress hormones and inflammatory mediators, i.e. cytokines, induce the so-called “Systemic Inflammatory Response Syndrome” (SIRS) which has a major impact on metabolism. SIRS causes hyperglycaemia and whole-body protein catabolism.
The elderly and frail. The elderly undergo surgery four times more often than the rest of the population, thus in the near future, a major proportion of patients presenting for surgery will be aged more than 65 years, with a substantial number older than 85 years (45). By extrapolating the impact of the ageing population, we should expect more than a 10% increase in the incidence of postoperative morbidity annually, with increased healthcare expenditure. This is underpinned by the fact that the population segment older than 80 years is expected to increase by 351% by 2050 (46). The frailty syndrome denotes age‑related multisystem physiological reserve decline, manifesting as increased vulnerability to minor stressors. Frailty is a validated and independent risk factor for complications (47).
Selecting the right patient – not so easy.
Since prehabilitation programs are resource intensive and can be time consuming, selection of the right program for the right patient remains one of the major challenges. For functional capacity, this is the Duke Activity Status Index (DASI), where a questionnaire of 12 questions estimates the functional capacity of the patient (48). Whereas the gold standard for measurement of the exercise capacity remains the CPET on a stationary bike as mentioned above. A poor nutritional status can be reliably identified with simple questionnaires such as the nutritional risk score (NRS) (49) or the Canadian Nutrition Screening Tool (CNST) (50), and can be further quantified with the Patient-Generated Subjective Global Assessment (PG-SGA) (51). Frailty is operationalized via the Fried phenotype (≥3 of 5 criteria) (52) or the Rockwood cumulative‑deficit frailty index (53). There are multiple tools to assess a patient for frailty (54). Most of these tools represent a composite of nutritional, physical and psychological deficiencies. Another challenge is integrating these simple tests into routine clinical practice.
Postpone surgery for Patient Optimization – are you mad?
Delaying elective procedures to allow for targeted preoperative optimization might enhance both clinical outcomes and patient experience. Especially high‑risk individuals, such as those with poor cardiopulmonary fitness, severe malnutrition, anemia or poorly-managed diabetes mellitus, benefit most from a brief postponement that enables tailored interventions like exercise-based prehabilitation, nutritional supplementation, anemia management, and smoking cessation programs (55). A very recent systematic review in patients undergoing major gastrointestinal oncological surgery (56), together with a meta-analysis on prehabilitation in frail patients (57), demonstrated that prehabilitation significantly reduces the rate of postoperative complications. On the other hand, retrospective studies, analyzing delays for cancer surgery during the Covid-19 pandemic, indicated that delays of weeks and even months did not compromise oncologic safety in cancer resections (58-62). This suggests that short delays do not worsen long‑term survival or cancer‑specific outcomes; rather, a short period of 2-4 weeks can be used to build resilience against the “surgical stress” response and decrease the likelihood of complications and prolonged recovery or loss of independence. In practice, thoughtful postponement—when balanced against disease urgency—ensures that patients proceed to surgery in the best possible condition, avoiding the downstream morbidity associated with “rushed” interventions.
Experiences from the ongoing PREHABIL trial at the Inselspital in Bern
The prospective, planned multicentre, multidisciplinary and multimodal PREHABIL started in early 2022 (63). The study initiated by two anesthesiologists and planned in cooperation with cardio-rehabilitation and nutrition experts as well as physical therapists, initially aimed to include over 450 patients over a period of 3 years. However, not everything worked out as planned. Despite broad endorsement from surgical colleagues across multiple specialties, recruitment has remained—and continues to be—the primary challenge for this SNSF‑supported trial. Despite initial optimism that surgeons would refer patients opportunistically following consultations which represents an important step in the process of prehabilitation, referral rates remained disappointingly low—even after daily reminders to every operating surgeon. To address this, the research team instituted proactive measures: a dedicated member now continuously screens surgical schedules, attends tumor board meetings, and invites eligible patients for cardiopulmonary exercise testing to identify those with low functional capacity for enrollment. As of now, half of our target cohort was enrolled in the first quarter of this year, with 2–3 new recruits per week. Since the trial has started, we demonstrated that simple preoperative physical activity monitoring significantly increases daily step counts in high‑risk non-cardiac surgery patients (64), and that tele‑supervised inspiratory muscle training is both feasible and effective in improving maximal inspiratory pressure (MIP) in elderly patients with low cardiopulmonary reserve (data not published yet). Further, to identify the challenges and facilitators of adherence among older participants in our multimodal prehabilitation program, colleagues from the Institute of Psychology, Faculty of Philosophy and Human Sciences conducted ten telephone interviews with patients enrolled in the PREHABIL project. In their final evaluation patients noticed real physical gains and felt mentally stronger, which kept their motivation and confidence high. Social support—from partners, family, friends, and the research staff—gave them helpful advice and a sense of care (65). Although the efficacy of our multimodal program in reducing postoperative complications remains under evaluation, preliminary findings show good patient acceptance and adherence. Most participants express enthusiasm about actively contributing to improved surgical outcomes. Furthermore, for many—especially those facing cancer surgery—the opportunity to engage in a structured prehabilitation regimen provides significant psychological support during a challenging period of their life.
Future directions
From prehab to rehab. Prehabilitation should not end once a patient is admitted for surgery. Therefore, in future projects, we plan to combine prehabilitation with targeted early rehabilitation (66). Early rehabilitation may even begin at the post-anaesthesia care unit, before patients are transferred to the ward (67). The main goal of early rehabilitation is to mobilize patients as quickly as possible after surgery.
Digital biomarkers in perioperative care. The rapid development of wearable technology offers opportunities for perioperative care (68). Physical activity, heart rate, heart rate variability, blood pressure, respiratory rate, and sleep patterns can be monitored continuously. These digital biomarkers can be used to detect patients that are at high risk for complications, to tailor and monitor prehabilitation programs, and to track postoperative recovery.
Large language models to assess postoperative complications. Furthermore, to monitor whether newly introduced prehabilitation interventions are able to lower complication severity and/or incidence, specialized large language models may play an important role in near future. As of today, the assessment of complications is time consuming and requires dedicated staff. Based on hospital discharge reports, in-hospital hosted large language models may automate this task in the future (69). Studies that evaluate the performance of these models compared to human based ratings are needed.
Exploring the cost-saving effect of prehabilitation. With the increasing financial pressure on Swiss hospitals, economic factors need to be considered for the successful implementation of prehabilitation. There is some evidence that prehabilitation has a cost-saving effect in the context of the English National Healthcare Service (70). The cost-saving effect was explained by the lower incidence of severe complications and the shorter length of hospital stay of the patients participating in prehabilitation. Whether a cost-saving effect can be observed in context of the Swiss healthcare system needs to be evaluated.
Conclusion
Ideally, perioperative care would be organized as a standardized pathway starting in the outpatient clinic when indication for surgery is made until the patient returns to his full functional recovery at home (71). Prehabilitation, an emerging concept to improve patients before the surgery, is unquestionably part of the solution to improve postoperative outcomes in patients with a low functional capacity. There are many obstacles and challenges for reaching this integrative approach to delivering care for "a single operation", and it is key that care providers focus on the bigger picture and not only on the surgical procedure alone. For this, it is crucial that the surgeons and anesthetists consider themselves as one perioperative team rather than isolated specialties.
- Lucas DJ, Pawlik TM. Quality improvement in gastrointestinal surgical oncology with American College of Surgeons National Surgical Quality Improvement Program. Surgery. 2014;155(4):593-601.
- Djaladat H, Katebian B, Bazargani ST, Miranda G, Cai J, Schuckman AK, et al. 90-Day complication rate in patients undergoing radical cystectomy with enhanced recovery protocol: a prospective cohort study. World journal of urology. 2017;35(6):907-11.
- Tevis SE, Kennedy GD. Postoperative complications and implications on patient-centered outcomes. J Surg Res. 2013;181(1):106-13.
- Moran J, Wilson F, Guinan E, McCormick P, Hussey J, Moriarty J. Role of cardiopulmonary exercise testing as a risk-assessment method in patients undergoing intra-abdominal surgery: a systematic review. Br J Anaesth. 2016;116(2):177-91.
- Lawrence VA, Hazuda HP, Cornell JE, Pederson T, Bradshaw PT, Mulrow CD, et al. Functional independence after major abdominal surgery in the elderly. Journal of the American College of Surgeons. 2004;199(5):762-72.
- Nicholson A, Lowe MC, Parker J, Lewis SR, Alderson P, Smith AF. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. The British journal of surgery. 2014;101(3):172-88.
- Stabenau HF, Becher RD, Gahbauer EA, Leo-Summers L, Allore HG, Gill TM. Functional Trajectories Before and After Major Surgery in Older Adults. Ann Surg. 2018;268(6):911-7.
- Grocott MP, Mythen MG. Perioperative Medicine: The Value Proposition for Anesthesia?: A UK Perspective on Delivering Value from Anesthesiology. Anesthesiology clinics. 2015;33(4):617-28.
- Armbrust R, Schneider S, Spies C, du Bois A, Sehouli J. Prehabilitation programs and ERAS protocols in gynecological oncology: a comprehensive review. Archives of gynecology and obstetrics. 2019.
- Iniesta MD, Lasala J, Mena G, Rodriguez-Restrepo A, Salvo G, Pitcher B, et al. Impact of compliance with an enhanced recovery after surgery pathway on patient outcomes in open gynecologic surgery. International journal of gynecological cancer : official journal of the International Gynecological Cancer Society. 2019.
- Liu JY, Wick EC. Enhanced Recovery After Surgery and Effects on Quality Metrics. The Surgical clinics of North America. 2018;98(6):1119-27.
- Bisch SP, Jago CA, Kalogera E, Ganshorn H, Meyer LA, Ramirez PT, et al. Outcomes of enhanced recovery after surgery (ERAS) in gynecologic oncology - A systematic review and meta-analysis. Gynecol Oncol. 2021;161(1):46-55.
- Spain J. Prehabilitation. Clin Sports Med. 1985;4(3):575-85.
- Teitz CC, Cook DM. Rehabilitation of neck and low back injuries. Clin Sports Med. 1985;4(3):455-76.
- PREHABILITATION, rehabilitation, and revocation in the Army. Br Med J. 1946;1:192-7.
- Ditmyer MM, Topp R, Pifer M. Prehabilitation in Preparation for Orthopaedic Surgery. Orthopaedic Nursing. 2002;21(5):43-54.
- Scheede-Bergdahl C, Minnella EM, Carli F. Multi-modal prehabilitation: addressing the why, when, what, how, who and where next? Anaesthesia. 2019;74 Suppl 1:20-6.
- Engel D, Furrer MA, Wuethrich PY, Loffel LM. Surgical safety in radical cystectomy: the anesthetist's point of view-how to make a safe procedure safer. World journal of urology. 2019.
- Santa Mina D, Clarke H, Ritvo P, Leung YW, Matthew AG, Katz J, et al. Effect of total-body prehabilitation on postoperative outcomes: a systematic review and meta-analysis. Physiotherapy. 2014;100(3):196-207.
- Moran J, Guinan E, McCormick P, Larkin J, Mockler D, Hussey J, et al. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: A systematic review and meta-analysis. Surgery. 2016;160(5):1189-201.
- Howard R, Yin YS, McCandless L, Wang S, Englesbe M, Machado-Aranda D. Taking Control of Your Surgery: Impact of a Prehabilitation Program on Major Abdominal Surgery. Journal of the American College of Surgeons. 2019;228(1):72-80.
- Gillis C, Buhler K, Bresee L, Carli F, Gramlich L, Culos-Reed N, et al. Effects of Nutritional Prehabilitation, With and Without Exercise, on Outcomes of Patients Who Undergo Colorectal Surgery: A Systematic Review and Meta-analysis. Gastroenterology. 2018;155(2):391-410.e4.
- Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS, et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc. 2013;27(4):1072-82.
- van Rooijen S, Carli F, Dalton S, Thomas G, Bojesen R, Le Guen M, et al. Multimodal prehabilitation in colorectal cancer patients to improve functional capacity and reduce postoperative complications: the first international randomized controlled trial for multimodal prehabilitation. BMC Cancer. 2019;19(1):98.
- Bos AC, van Erning FN, van Gestel YR, Creemers GJ, Punt CJ, van Oijen MG, et al. Timing of adjuvant chemotherapy and its relation to survival among patients with stage III colon cancer. European journal of cancer (Oxford, England : 1990). 2015;51(17):2553-61.
- Carli F, Silver JK, Feldman LS, McKee A, Gilman S, Gillis C, et al. Surgical Prehabilitation in Patients with Cancer: State-of-the-Science and Recommendations for Future Research from a Panel of Subject Matter Experts. Physical medicine and rehabilitation clinics of North America. 2017;28(1):49-64.
- Engel D, Testa GD, McIsaac DI, Carli F, Santa Mina D, Baldini G, et al. Reporting quality of randomized controlled trials in prehabilitation: a scoping review. Perioper Med (Lond). 2023;12(1):48.
- McIsaac DI, Gill M, Boland L, Hutton B, Branje K, Shaw J, et al. Prehabilitation in adult patients undergoing surgery: an umbrella review of systematic reviews. Br J Anaesth. 2022;128(2):244-57.
- Feldman LS, Carli F. From Preoperative Assessment to Preoperative Optimization of Frailty. JAMA surgery. 2018;153(5):e180213.
- Lukez A, Baima J. The Role and Scope of Prehabilitation in Cancer Care. Seminars in oncology nursing. 2020;36(1):150976.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018;68(6):394-424.
- Older PO, Levett DZH. Cardiopulmonary Exercise Testing and Surgery. Ann Am Thorac Soc. 2017;14(Supplement_1):S74-S83.
- Mazur A, Brat K, Homolka P, Merta Z, Svoboda M, Bratova M, et al. Ventilatory efficiency is superior to peak oxygen uptake for prediction of lung resection cardiovascular complications. PLoS One. 2022;17(8):e0272984.
- Shafiek H, Valera JL, Togores B, Torrecilla JA, Sauleda J, Cosío BG. Risk of postoperative complications in chronic obstructive lung diseases patients considered fit for lung cancer surgery: beyond oxygen consumption. Eur J Cardiothorac Surg. 2016;50(4):772-9.
- Brunelli A, Belardinelli R, Pompili C, Xiumé F, Refai M, Salati M, et al. Minute ventilation-to-carbon dioxide output (VE/VCO2) slope is the strongest predictor of respiratory complications and death after pulmonary resection. Ann Thorac Surg. 2012;93(6):1802-6.
- Tolchard S, Angell J, Pyke M, Lewis S, Dodds N, Darweish A, et al. Cardiopulmonary reserve as determined by cardiopulmonary exercise testing correlates with length of stay and predicts complications after radical cystectomy. BJU Int. 2015;115(4):554-61.
- Carlisle J, Swart M. Mid-term survival after abdominal aortic aneurysm surgery predicted by cardiopulmonary exercise testing. The British journal of surgery. 2007;94(8):966-9.
- Vaid S, Bell T, Grim R, Ahuja V. Predicting risk of death in general surgery patients on the basis of preoperative variables using American College of Surgeons National Surgical Quality Improvement Program data. The Permanente journal. 2012;16(4):10-7.
- Kwag SJ, Kim JG, Kang WK, Lee JK, Oh ST. The nutritional risk is a independent factor for postoperative morbidity in surgery for colorectal cancer. Annals of surgical treatment and research. 2014;86(4):206-11.
- Sun Z, Kong XJ, Jing X, Deng RJ, Tian ZB. Nutritional Risk Screening 2002 as a Predictor of Postoperative Outcomes in Patients Undergoing Abdominal Surgery: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. PLoS One. 2015;10(7):e0132857.
- Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, et al. Risk factors for 30-day hospital readmission among general surgery patients. Journal of the American College of Surgeons. 2012;215(3):322-30.
- Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN guideline: Clinical nutrition in surgery. Clin Nutr. 2017;36(3):623-50.
- Gillis C, Wischmeyer PE. Pre-operative nutrition and the elective surgical patient: why, how and what? Anaesthesia. 2019;74 Suppl 1:27-35.
- Gillis C, Carli F. Promoting Perioperative Metabolic and Nutritional Care. Anesthesiology. 2015;123(6):1455-72.
- Aubrun F, Gazon M, Schoeffler M, Benyoub K. Evaluation of perioperative risk in elderly patients. Minerva anestesiologica. 2012;78(5):605-18.
- Schier R, Levett D, Riedel B. Prehabilitation: The next challenge for anaesthesia teams. European journal of anaesthesiology. 2020;37(4):259-62.
- Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC, Jr., Moss M. Simple frailty score predicts postoperative complications across surgical specialties. American journal of surgery. 2013;206(4):544-50.
- Wijeysundera DN, Pearse RM, Shulman MA, Abbott TEF, Torres E, Ambosta A, et al. Assessment of functional capacity before major non-cardiac surgery: an international, prospective cohort study. Lancet. 2018;391(10140):2631-40.
- Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321-36.
- Laporte M. The Canadian Nutrition Screening Tool. Adv Skin Wound Care. 2017;30(2):64-5.
- Bauer J, Capra S, Ferguson M. Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr. 2002;56(8):779-85.
- McIsaac DI, MacDonald DB, Aucoin SD. Frailty for Perioperative Clinicians: A Narrative Review. Anesthesia and analgesia. 2020;130(6):1450-60.
- Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722-7.
- Aucoin SD, Hao M, Sohi R, Shaw J, Bentov I, Walker D, et al. Accuracy and Feasibility of Clinically Applied Frailty Instruments before Surgery: A Systematic Review and Meta-analysis. Anesthesiology. 2020;133(1):78-95.
- Barberan-Garcia A, Ubré M, Roca J, Lacy AM, Burgos F, Risco R, et al. Personalised Prehabilitation in High-risk Patients Undergoing Elective Major Abdominal Surgery: A Randomized Blinded Controlled Trial. Ann Surg. 2018;267(1):50-6.
- Ambulkar R, Kunte A, Solanki SL, Thakkar V, Deshmukh B, Rana PS. Impact of Prehabilitation in Major Gastrointestinal Oncological Surgery: a Systematic Review. J Gastrointest Cancer. 2025;56(1):133.
- Bai Z, Koh C, Solomon M, Shahab R, Hirst N, Alexander K, et al. Prehabilitation in Frail Patients Undergoing Cancer Surgery: A Systematic Review and Meta-analysis. Annals of Surgical Oncology. 2025.
- Trepanier M, Paradis T, Kouyoumdjian A, Dumitra T, Charlebois P, Stein BS, et al. The Impact of Delays to Definitive Surgical Care on Survival in Colorectal Cancer Patients. J Gastrointest Surg. 2020;24(1):115-22.
- Brugel M, Bouché O, Kianmanesh R, Teuma L, Tashkandi A, Regimbeau JM, et al. Time from first seen in specialist care to surgery does not influence survival outcome in patients with upfront resected pancreatic adenocarcinoma. BMC Surg. 2021;21(1):413.
- Xu K, Watanabe-Galloway S, Rochling FA, Farazi PA, Monirul Islam KM, Wang H, et al. Surgical Delay Is Associated with Improved Survival in Hepatocellular Carcinoma: Results of the National Cancer Database. J Gastrointest Surg. 2019;23(5):933-43.
- Ma J, Zhu C, Li W, Qiu Z, Yang J, Ge L, et al. The Effect of Delayed Oncology Surgery on Survival Outcomes for Patients With Gastric Cancer During the COVID-19 Pandemic: Evidence-Based Strategies. Front Oncol. 2022;12:780949.
- Turaga KK, Girotra S. Are We Harming Cancer Patients by Delaying Their Cancer Surgery During the COVID-19 Pandemic? Ann Surg. 2023;278(5):e960-e5.
- Beilstein CM, Krutkyte G, Vetsch T, Eser P, Wilhelm M, Stanga Z, et al. Multimodal prehabilitation for major surgery in elderly patients to lower complications: protocol of a randomised, prospective, multicentre, multidisciplinary trial (PREHABIL Trial). BMJ Open. 2023;13(1):e070253.
- Vetsch T, Dueblin SW, Eser P, Beilstein CM, Wuethrich PY, Wilhelm M, et al. Effect of multimodal home-based prehabilitation on objectively measured physical activity in patients undergoing elective cardiac or non-cardiac major surgery: secondary outcomes from a randomised controlled trial. Perioper Med (Lond). 2025;14(1):69.
- Ramona Thöny DCB. Die Herausforderungen und Ressourcen der Adhärenz bei Teilnehmenden eines multimodalen Prähabilitationsprogramms 2024 [Available from: https://www.gpv.psy.unibe.ch/forschung/index_ger.html.
- Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. 2022;11(2):121-9.
- Pastene B, Labarriere A, Lopez A, Charvet A, Culver A, Fiocchi D, et al. Ultra-early initiation of postoperative rehabilitation in the post-anaesthesia care unit after major thoracic surgery: case-control study. BJS Open. 2022;6(3).
- Lu JK, Wang W, Mahadzir MDA, Poganik JR, Moqri M, Herzog C, et al. Digital biomarkers of ageing for monitoring physiological systems in community-dwelling adults. Lancet Healthy Longev. 2025;6(6):100725.
- Staubli SM, Walker HL, Saner F, Salinas CH, Broering DC, Malagò M, et al. Decoding the Clavien-Dindo Classification: Artificial Intelligence (AI) as a Novel Tool to Grade Postoperative Complications. Ann Surg. 2024.
- Bernarda Zamora Zamora Talaya KM, Katerina Savva. A health economic model to assess the impact of prehabilitation on hospital cost savings in gastrointestinal cancer, modelled on English National Health Service tariff. 2023 ASCO Annual Meeting Journal of Clinical Oncology; 2023.
- Levy N, Grocott MPW, Carli F. Patient optimisation before surgery: a clear and present challenge in peri-operative care. Anaesthesia. 2019;74 Suppl 1:3-6.
- Davis JF, van Rooijen SJ, Grimmett C, West MA, Campbell AM, Awasthi R, et al. From Theory to Practice: An International Approach to Establishing Prehabilitation Programmes. Curr Anesthesiol Rep. 2022;12(1):129-37.
- Engel D, Furrer MA, Wuethrich PY, Löffel LM. Surgical safety in radical cystectomy: the anesthetist's point of view—how to make a safe procedure safer. World journal of urology. 2020;38(6):1359-68.