Robotic surgery is growing in popularity worldwide, with the global market estimated to reach $20 billion by 2024. Similarly, in Europe, robotic surgery is becoming increasingly prominent, with the UK, Germany and Spain leading the way. In Switzerland, robotic surgery is also becoming a preferred practice in many medical institutions, allowing surgeons to perform complex, precise operations with great accuracy and precision and less risk of complications than ever before.1,2 Therefore, institutions invested in robotic surgical technology to ensure best possible care. As a result, robotic surgery is increasingly available in many of Switzerland‘s leading hospitals, a trend that will continue in the future with expanding applications and more complex procedures. Regarding educational aspects, robotic surgery may limit the opportunity for surgical residents to obtain first-hand experience during procedures, which is one of the key concerns.
This is so that the resident can frequently observe or assist „from a distance“ while the more experienced surgeons perform the robotic operation, sitting on the console. Therefore, robotic surgery may demand a different set of abilities and methods than conventional open surgery or even laparoscopic surgery, which may result in a change in the nature of surgical procedures and the talents needed to accomplish them.
The technology of robotic surgery offers several advantages over conventional open or laparoscopic surgery. Robot-assisted surgery provides increased accuracy and precision, reduced blood loss,
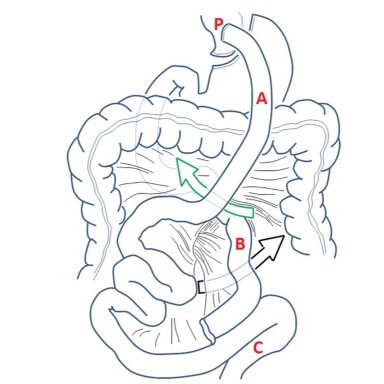
lower risk of infection and faster recovery times with a shorter hospital stay than open surgery.3–5 Ultimately, randomized-controlled trials started to show that robotic surgery resulted in better oncological quality of resection than conventional laparoscopic surgery, with less surgical trauma, and better postoperative recovery.4 However, the transition from open to robotic surgery comes with a learning curve.6,7 If not trained appropriately, several technical difficulties and serious complications can be experienced during the establishment of robotic complex procedures.8,9 Also, the transferability of skills from established open and laparoscopic surgery is controversial as the robotic surgery approach differs from others.10 However, there has never been such a one-to-one teaching situation in surgery with the same perspective and „hands“ as the robot offers unprecedented opportunities for both the supervisor and the resident: two consoles with the same intraoperative situs, pointing instruments (digitally blue arrow on the screen) or the surgical supervisor can even use the fourth arm of the robot.
Most robotic surgeries are only performed by highly trained professionals, while the education on the robotic platform is guided and organized by the robotic companies, which we as surgical
educators see as problematic. Also, the rate of robots sold in Switzerland (and worldwide) is increasing tremendously, and a one-on-one training by the company can no longer be carried out
to cover the needs. The industry-driven programmes are also just device trainings without sufficient medical expertise. In fact, many consider a basic class in how to handle a robot as sufficient to be considered "robot ready", although no specific operation is taught in these company-based courses.
To ensure a comprehensive approach to using robotic surgery, the establishment of an appropriate training program is crucial – one example being the LEALPS 3 (Outcomes of a Multicenter Training
Program in Robotic Pancreatoduodenectomy).11 Hence, systematic, competency-based training from surgeons to surgeons is desperately needed! Entrustable Professional Activities (EPAs) such as procedural EPAs in robotic surgery have the potential to significantly improve the implementation of robotics in abdominal surgery. EPAs are clinical tasks that medical learners or trainees can be trusted to perform with maximum over minimal to no supervision.12 EPAs are an effort to define the competencies necessary for clinical practice and are used to assess and certify the readiness of learners to practice independently.
In general surgery, EPAs can be used to measure the competency of trainees in the performance of core surgical procedures, such as wound closure, laparoscopy, and endoscopy. EPAs
can also be used to assess how well learners are able to handle complex and challenging clinical scenarios, such as trauma resuscitation and management of post-operative complications.13 Additionally, EPAs can be used to evaluate the effectiveness of communication and team collaboration involved in surgical care.14,15
Safe training and proctoring of robotic surgery are possible and the learning curve can be substantially reduced by the following strategies:
- Utilizing simulation and dry-lab training to practice and refine techniques and important surgical steps such as suturing of anastomoses.16
- Increasing the number of robotic procedures supervised by an expert early-on in training, allowing the surgeon to become more familiar with the technology and the technique.17
- Use of the real-time image guided system, which provides feedback on the surgical procedure (different from laparoscopic or conventional procedures).18
- Incorporating team-based training, where surgeons and other support staff can practice and develop skills together (emergency conversion training).18
- Implementing EPAs as a frequent feedback opportunity to improve performances and satisfaction and ultimately define the learning standards and curve in order to steep the learning curve.19
Why exactly the learning curve? The learning curve in surgery is a graphical representation of the relationship between the accumulated experience of a surgeon and the quality of their performance.
It shows the rate at which a surgeon becomes more proficient in performing a procedure over time. Generally, the more experience surgeons have, the more skilled they become, thus demonstrating
a steep learning curve. However, the learning curve, even if declared as a relevant quality tool for educational programs in surgery, lacks standardization.6 Surgeons usually compare numbers,
e.g., numbers of procedures needed, operative time, blood loss, length of hospital stay of patients to define the learning curve but don’t consider competency-based surgical education, which will
be problematic within the future implementation of EPAs in surgery.
Therefore, we have to consider all educational options in order to define “the learning curve” and to maximize the surgical quality for the implementation of robotic surgery in times of resource
constraints and restricted working hours – especially in our role as “early-adopters” of EPAs in Switzerland. As surgical educators, we should set the standard for educating the next generation of
surgeons, not an industry company. Structured training programs are necessary to improve the learning curve and ultimately to ensure patient safety. The fact that the company has provided training exclusivity of the robot is no longer the case and needs to be made accessible to a broader audience. It is, therefore, the duty of every institution to ensure safe training.
EPAs can improve assessment of surgeons’ skills of the robotic approach while reducing the number of operations required to achieve safe mastery for robotic surgery. EPA is a framework for assessing the readiness of a practitioner to perform a certain task or activity. It consists of a structured set of criteria and performance standards for a specific activity. By providing a clear set of expectations
and standards, EPA can help steepen the learning curve for robotic surgery. The EPAs will include Robotic Surgery-specific tasks such as patient selection, the robotic system setup, patient
positioning, robotic arm manipulation, suturing, operating in planes or wound closure. Further challenges such as hand-foot-eye coordination, dealing with narrow space, or enlargement effect will be depicted in the EPA, allowing the trainees to gain the necessary skills and experience to perform robotic surgery safely and effectively.
Future
As the use of robotic surgery continues to increase, there may be a greater demand for training programs that specifically focus on the use of robotic technology. This could require additional resources and funding for residency programs. Robotic surgery may also require specialized training that is not typically included in traditional surgical residency programs. This could mean that surgical
residents will need to seek out additional training opportunities to gain the necessary skills and expertise. Others argue that robotic surgery may actually offer improved educational opportunities
for surgical residents, while the usage of robotic technology could allow for more detailed and precise visualization of surgical procedures, which could enhance the learning experience for residents. On the other hand, implementing EPAs in surgical practice will be the educational challenge in the next few years, not only in robotic surgery. The focus on numbers involved in the learning curve might be here the biggest challenge for surgical educators. Once EPAs have been developed and implemented, we then have to develop comprehensive programs for evaluating the competency of learners in each EPA.
Overall, the impact of robotic surgery on the teaching of surgical residents is a complex issue with both potential benefits and drawbacks. It will be important for residency programs to carefully
consider the implications of this technology and adapt their training programs accordingly to ensure that residents are well-prepared to meet the evolving demands of modern surgical practice.
Références
- Are robot-surgeons set to take over in Geneva? https://www.swissinfo.ch/eng/sci-tech/future-medicine_are-robot-surgeons-set-to-take-over-in-geneva-/41538890.
- What if your future surgeon were a robot? https://www.swissinfo.ch/eng/sci-tech/what-if-your-future-surgeon-were-a-robot-/46751924.
- Micha JP, Rettenmaier MA, Bohart RD, Goldstein BH. Robotic-Assisted Surgery for the Treatment of Breast and Cervical Cancers. JSLS. 2022;26(2):e2022.00014. doi:10.4293/JSLS.2022.00014
- Feng Q, Yuan W, Li T, et al. Robotic versus laparoscopic surgery for middle and low rectal cancer (REAL): short-term outcomes of a multicentre randomised controlled trial. The Lancet Gastroenterology & Hepatology. 2022;7(11):991-1004. doi:10.1016/S2468-1253(22)00248-5
- Seto Y, Mori K, Aikou S. Robotic surgery for esophageal cancer: Merits and demerits. Ann Gastroenterol Surg. 2017;1(3):193-198. doi:10.1002/ags3.12028
- Müller PC, Kuemmerli C, Cizmic A, et al. Learning Curves in Open, Laparoscopic, and Robotic Pancreatic Surgery: A Systematic Review and Proposal of a Standardization. Annals of Surgery Open. 2022;3(1):e111. doi:10.1097/AS9.0000000000000111
- Noh GT, Han M, Hur H, et al. Impact of laparoscopic surgical experience on the learning curve of robotic rectal cancer surgery. Surg Endosc. 2021;35(10):5583-5592. doi:10.1007/s00464-020-08059-5
- Alemzadeh H, Raman J, Leveson N, Kalbarczyk Z, Iyer RK. Adverse Events in Robotic Surgery: A Retrospective Study of 14 Years of FDA Data. Lee HS, ed. PLoS ONE. 2016;11(4):e0151470. doi:10.1371/journal. pone.0151470
- Gall TMH, Alrawashdeh W, Soomro N, White S, Jiao LR. Shortening surgical training through robotics: randomized clinical trial of laparoscopic versus robotic surgical learning curves. BJS Open. 2020;4(6):1100-1108. doi:10.1002/bjs5.50353
- Chahal B, Aydın A, Amin MSA, et al. Transfer of open and laparoscopic skills to robotic surgery: a systematic review. J Robotic Surg. Published online November 22, 2022. doi:10.1007/s11701-022-01492-9
- Zwart MJW, Nota CLM, de Rooij T, et al. Outcomes of a Multicenter Training Program in Robotic
Pancreatoduodenectomy (LAELAPS-3). Annals of Surgery. 2022;276(6):e886-e895. doi:10.1097/
SLA.0000000000004783 - Ten Cate O, Taylor DR. The recommended description of an entrustable professional activity: AMEE Guide No. 140. Medical Teacher. 2021;43(10):1106-1114. doi:10.1080/0142159X.2020.1838465
- Marty A, Frick S, Bruderer Enzler H, Zundel S. An analysis of core EPAs reveals a gap between curricular expectations and medical school graduates’ self-perceived level of competence. BMC Med Educ. 2021;21(1):105. doi:10.1186/s12909-021-02534-w
- Valding B, Monti M, Junod Perron N, et al. Entrustable professional activities for residency in general internal medicine: a systematic review: Swiss Med Wkly. 2022;152(4344):40002. doi:10.57187/smw.2022.40002
- Tørring B, Gittell JH, Laursen M, Rasmussen BS, Sørensen EE. Communication and relationship dynamics in surgical teams in the operating room: an ethnographic study. BMC Health Serv Res. 2019;19(1):528. doi:10.1186/s12913-019-4362-0
- Willuth E, Hardon SF, Lang F, et al. Robotic-assisted cholecystectomy is superior to laparoscopic cholecystectomy in the initial training for surgical novices in an ex vivo porcine model: a randomized crossover study. Surg Endosc. 2022;36(2):1064-1079. doi:10.1007/s00464-021-08373-6
- de Rooij T, van Hilst J, Boerma D, et al. Impact of a Nationwide Training Program in Minimally Invasive Distal Pancreatectomy (LAELAPS). Annals of Surgery. 2016;264(5):754-762. doi:10.1097/SLA.0000000000001888
- Unberath M, Gao C, Hu Y, et al. The Impact of Machine Learning on 2D/3D Registration for Image-Guided Interventions: A Systematic Review and Perspective. Front Robot AI. 2021;8:716007. doi:10.3389/frobt.2021.716007
- Berger S, Stalmeijer RE, Marty AP, Berendonk C. Exploring the Impact of Entrustable Professional Activities on Feedback Culture: A Qualitative Study of Anesthesiology Residents and Attendings. Academic Medicine. 2023;Publish Ahead of Print. doi:10.1097/ACM.0000000000005188