Unmasking the uncommon
The challenge of a „zebra“ in proctology

a publication of the Swiss College of Surgeons
Dossier
Ein Bilderrätsel und seine Auflösung: Wir stellen eine Frage aus dem chirurgischen Alltag und beantworten sie.
A Case of Intestinal Obstruction of Uncertain Etiology
A mystery in the bursa (Latin: bag, sac) caused moderate clinical signs yet led to major abdominal surgery. We present a diagnosis with a plethora of nonspecific symptoms that poses a diagnostic challenge for both surgeons and radiologists.
A 38-year old female presented to the emergency department with a one-day history of acute pain in the upper right quadrant of the abdomen, increasing within the last few hours. Her medical history included a non-alcoholic fatty liver disease with moderate hepatic fibrosis, endometriosis and hypertension.

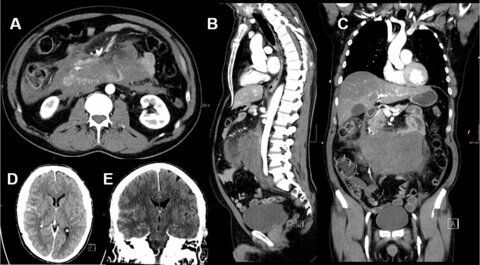
This 58-year-old male patient with no prior medical or surgical history (no medication, no substance abuse) was sitting at dinner with his wife, when he suddenly felt epigastric pain and upon standing up, lost consciousness, fell and hit his head on the floor. He regained consciousness upon arrival of the ambulance and, except for disorientation, was neurologically not impaired.
The incidence of acute mesenteric ischaemia (AMI) is very low, accounting for approximately 0.1-0.2% of all surgical admissions (1). However, if left untreated, mortality is high at 50% (2).

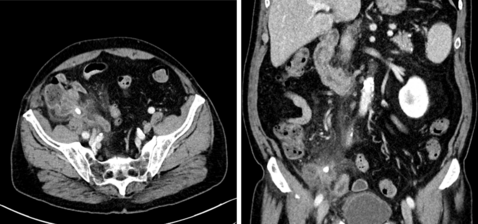
An 80-year-old male patient presented to the emergency department with a one-day history of right lower quadrant abdominal pain with no associated nausea or vomiting. He had similar symptoms for which he underwent appendectomy 60 years ago.
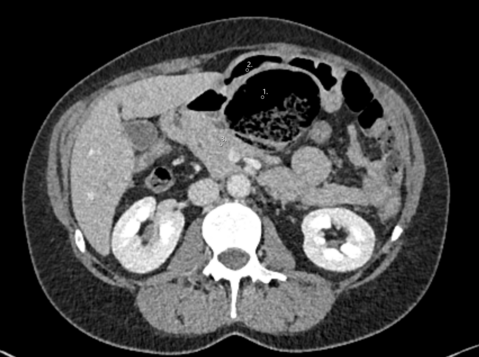
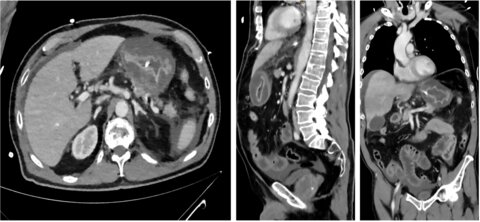
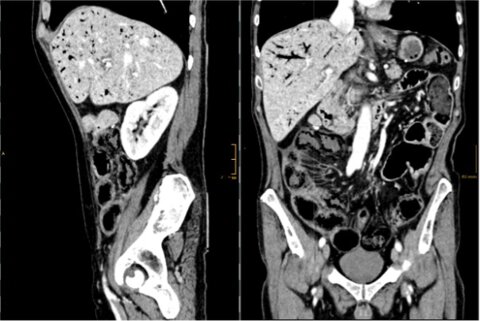
A 70-year-old male patient presented to the emergency department with a 4-day history of abdominal pain, vomiting, constipation and nausea. Similar episodes in the past year resolved after dietary modifications.

A 76-year-old patient presented in septic shock with diffuse abdominal pain two days after upper endoscopy. Fluid resuscitation and broad-spectrum antibiotics were administered. Initial diagnostics revealed an enlarged stomach wall. After further detoriation and development of an abdominal compartment syndrome a partial gastrectomy and open-abdomen treatment was performed.
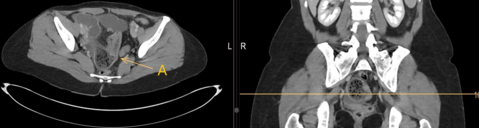
An 89-year-old-woman with a history of hysterectomy presented to the emergency department with a sudden onset of pelvic pressure and vaginal prolapse.

A 52-year-old man presented to the emergency department with acute abdominal pain and bloody tinged output through the stoma.
A 78-year-old male patient presented to the emergency department with absent bowel movements for 4 days and increasing abdominal pain and cramps.
