Methods:
An international panel of 15 pediatric surgeons from 9 countries went through a structured process consisting of a rapid scoping review, iterative discussion sessions, mixed-methods studies with key stakeholders, and voting rounds on individual statements to create draft consensus statements.
Results:
100 articles were identified during the review and summarized by application. Based on this condensed evidence, consensus statements were generated after 3 iterative rounds of anonymous voting. Key areas of agreement were quality of evidence, the safety of ICG, pediatric surgical indications, utilization per surgical specialty, and dosing of ICG.
Conclusion:
This consensus statement aims to guide healthcare professionals in managing ICG-SF use in pediatric surgery based on the best available evidence, key stakeholder consultation, and expert opinions. Despite the promising potential of ICG-FS, the need for higher-quality evidence, prospective trials, and safety studies is underscored. The consensus also provides support for pediatric surgeons to facilitate the application of ICG-FS.
Key words: indocyanine green fluorescence, tissue perfusion, immunofluorescence, pediatric surgery, fluorescence-guided surgery
Introduction
Indocyanine Green (ICG) is a water-soluble, tricarbocyanine with a high binding affinity to plasma proteins and excitation and emission spectra in the near-infrared (NIR) range1,2.
ICG-fluorescence imaging (ICG-F) applications have expanded to various surgical fields, including oncological surgery, neurosurgery, and gastrointestinal surgery. It aids in intraoperative visualization, tissue perfusion assessment, and lymphatic mapping.
The evidence base for ICG-F use in pediatric surgery is primarily built on small-scale, retrospective studies, highlighting the need for high-quality, prospective research to confirm its potential and explore new applications3. While ICG-F is very promising, it remains unclear whether its use improves surgical outcomes in the pediatric population.
The assembled consensus group proposed a set of guidelines for using ICG-F in pediatric surgery. Central issues such as the quality of current evidence, safety of ICG, specific pediatric indications, application across surgical specialties, and dosing strategies are addressed. We hypothesize that ICG-F can facilitate surgical procedures, improve decision-making, and decrease complications in pediatric surgery. This consensus statement offers clinicians, researchers, and surgeons an authoritative reference point for using ICG-F in pediatric surgery.
Methods
Literature Review
PubMed was systematically searched via a scoping review (intended to map the existing literature on a specific topic quickly)4–6 for articles on the use of ICG-F in pediatric surgery. The review aimed to identify, categorize, and summarize relevant publications to provide insights into current practices, clinical outcomes, and gaps in the existing body of evidence. Standardized data extraction forms were used across all topics. A uniform Excel database template for entering the data extracted from the selected papers was provided to all participants.
Development of the Consensus Process
The methods for developing our pediatric surgery consensus statement involved a three-round Delphi process with 15 expert pediatric surgeons, each with over 5 years of post-qualification experience, selected via snowball and purposive sampling.
The Internal Review Board approved the study (IRB- 00002938). Initially, panelists responded to questions based on their professional expertise and stakeholder input (Supplement 2). The second round involved reviewing the literature to determine clinical consensus needs and address discrepancies. Panelists reviewed these findings to agree upon or adjust recommendations.
Panelists voted on each consensus statement via a RedCap™ survey, expressing agreement, disagreement, or neutrality. The process repeated until at least 80% agreement was achieved on each statement. Recommendations surpassing this threshold are reported,
Each article reviewed was assigned a level of evidence using the original Center for Evidence-Based Medicine levels (http://www.cebm.net/ocebm-levels-of-evidence/) and graded as 'strong', 'weak', or 'no recommendation' according to the GRADE system. Statements with sufficient data received a grade of recommendation (GoR)7.
Results and Consensus Recommendations
Quality of Evidence
The initial search identified 558 titles, from which 77 abstracts were screened, 46 were located by additional methods, and 100 full-text papers were reviewed. The included studies are diverse, comprising 41 case reports, 18 case series, 21 retrospective studies, 13 prospective studies, and 7 others of various types. The panel unanimously agreed on the need for high-quality research and standardized ICG-F results reporting.
Safety of ICG
In the pediatric population, in a combined study of 75 (45 receiving ICG-F) patients evaluating gastrointestinal perfusion, no complications were noted9. A recent Pediatric Health Information System database study of ICG-F in pediatrics between 2016 and 2021 in 1270 cases across 38 participating hospitals demonstrated no adverse events10. Of the 100 articles reviewed, 44 did not provide any safety information, and 56 articles reported no ICG-related complications except two cases of temporary skin color change from dermal ICG administration11,12.
Regarding the safety profile ICG-F utilization has demonstrated a favorable safety profile, including very young/small patients with rare allergic reactions. However, data on pediatric safety reporting remains limited. We recommend strongly that ICG-F has a positive safety record.
Indocyanine Green Fluorescence in Pediatric Surgical Applications
ICG-F continues to have an expanded role in pediatric surgery, enhancing real-time visualization across applications such as tumor visualization, perfusion assessment, visual assessment of anatomical structures, and lymphatic mapping, among other clinical utilities.
Tumor Visualization and tumor margin identification
In tumor visualization and margin identification, 22 articles highlighted the efficacy of ICG-F for both primary and metastatic tumors13–34. ICG-F’s application in malignancies like bone tumors, soft tissue sarcomas, and Wilms tumor is still being evaluated. For oncologic procedures, ICG-F typically involves a larger dose of ICG given 24 hours or more beforehand, capitalizing on the "enhanced permeability and retention effect" where dye washes out from normal tissues but remains in tumor tissues during this “second window.” Notably, Harris (2023)20 reported the safe and effective use of ICG in minimally invasive surgery for pediatric oncology, and Kitagawa (2015)21 highlighted its efficacy in identifying hepatoblastoma pulmonary metastases. Shen's study (2023)25, analyzing 23 pediatric hepatoblastoma resections using ICG-F, found the technique invaluable for margin identification and reducing residual tumor risk. Thus, efficacy in Tumor Visualization ICG-F can significantly enhance the visualization of hepatic tumors, especially in metastatic settings, and play a pivotal role in delineating tumor margins.
The effectiveness of ICG-F for bone tumors, soft tissue sarcomas, and Wilms tumor remains under evaluation. ICG-F is both safe and effective in minimally invasive surgeries for pediatric oncology patients. ICG-F is an encouraging, emerging technology for tumor visualization and margin identification in pediatric oncological surgery. ICG-F significantly improves tumor visualization in hepatic and hepatoblastoma settings. Its efficacy for visualization of other tumors is more variable and remains under investigation. A more robust evidence base achieved through rigorous scientific research is needed to confirm these preliminary findings and to guide its integration into clinical practice protocols. ICG administration timing is based on the difference in the assessment goal desired (perfusion vs. retention).
Perfusion Assessment
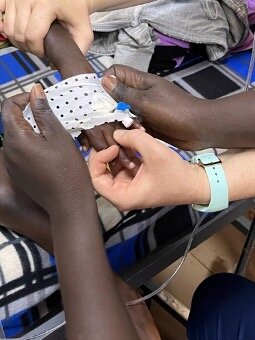
In 31 articles, ICG-F effectively assessed tissue for bowel, esophagus, abdominal wall, skin flap etc. perfusion35–63. Through monitoring ICG-F, surgeons identified compromised perfusion, enabling timely interventions to reduce ischemic risks. Le-Nguyen et al. (2023)51 conducted a prospective study of 28 pediatric intestinal resections using ICG-F, including 14 patients from the NICU. They found that ICG-F may impact bowel resection sites by improving perfusion assessment and demonstrated a very favorable safety profile, even for very small patients. ICG-FA is a potential intraoperative tool for real-time tissue perfusion assessment, current non-randomized data supports ICG-FA's safety and efficacy in pediatric surgeries. Still, robust randomized trials are essential to determine if this impacts complications such as rates of anastomotic leak or stricture.
Visualization Enhancement
ICG-F enhances intra-operative visualization, aiding surgeons in identifying key structures such as anatomic structures, vessels, and tumors (Table 2). Of 28 articles that were identified11,64–86, seven were prospective clinical studies. Esposito et al. compared laparoscopic partial nephrectomy with and without ICG-F in 40 patients, finding that clearer vessels and renal visualization reduced operative time71. Esposito et al. (2020)87 confirmed ICG-F imaging effectiveness and safety in pediatric minimally invasive surgery for abdominal lymphoma and ovarian tumors. A review by Esposito et a. (2022) showed that ICG-F enhances surgical visualization in urologic oncology procedures, particularly through tumor inverse pattern of ICG-F visualization (hypo visualization of tumors). Therefore, ICG-F enhances visualization in pediatric surgery via contrasting tissues, enhancing the visibility of vessels, anatomic structures, and tumors. Preliminary findings suggest ICG-F's may reduce operative time and complications related to anatomic visualization.
Lymphatic System and Lymphatic Mapping
Lymphatic mapping is essential for staging and surgical management in certain pediatric malignancies but carries morbidity. 16 articles described lymphatic drainage pathway mapping facilitated by ICG-F, aiding in the identification and excision of sentinel lymph nodes12,26,47–49,64,88–97. ICG-F reduced unnecessary lymphadenectomies and related complications. Jeremiasse et al. (2023)91 reported ICG-F’s feasibility for imaging the sentinel lymph node during pediatric melanoma, squamous cell carcinoma, or sarcoma cases, noting superior detection rate and accuracy. Kato et al. (2019)92, studied lymphatic malformations and found ICG-F useful in identifying and guiding the treatment of lymph flow patterns in refractory lymphatic malformation. Mansfield et al. (2020)93 compared the outcomes of retroperitoneal lymph node dissection (RPLND) for para testicular rhabdomyosarcoma concluding that a retroperitoneoscopic approach, combined with ICG-F enhanced outcomes. Thus, ICG-F-assisted lymphatic mapping is a promising tool in enhancing the surgical approach to pediatric malignancies. Existing literature affirms the safety and effectiveness of ICG-F for sentinel lymph node detection, but comparative prospective trials are required to ascertain ICG-F's advantage over conventional techniques. Implementing ICG-F for lymphatic mapping may diminish complication risks by obviating certain lymphadenectomy s and enabling precise lymph node operations. ICG-F may be applicable for congenital lymphatic malformation resection cases.
Fluorescence Cholangiography
In total, 23 articles describing the application of ICG-F in hepato-pancreato-biliary surgery17,23,25,28,29,31–33,37,41,50,65–67,73–75,77,78,84,86 covering procedures such as laparoscopic cholecystectomy, Kasai procedure, and partial hepatectomy. Calabro et al. (2020)66 studied the effects of ICG-F cholangiography (ICG-FC) during laparoscopic cholecystectomy in 50 pediatric patients, finding it safe and effective for biliary tree identification. Esposito et al. published two retrospective studies in 2019 and 202267,72. The first analyzed 215 children’s long-term outcomes after laparoscopic cholecystectomy, showing its long-term safety and effectiveness. The 2022 study on 43 patients compared standard laparoscopic cholecystectomy to ICG-FC cholecystectomy. ICG-FC enhanced visualization and reduced specific operative step time, but overall operative time and hospital stay were insignificant between the comparative groups. ICG-F is a safe and potentially effective instrument for a range of hepatobiliary operations within the pediatric population. ICG-F may even become mandatory for standard procedures such as cholecystectomy.
Pediatric colorectal and pelvic reconstructive surgery
ICG-F is increasingly utilized in pediatric colorectal and pelvic reconstruction surgeries46,54,59,63, aiding in repairs like anorectal malformations, Hirschsprung disease, and complex reoperations. It proves useful for evaluating tissue perfusion in structures such as the neovagina and colon and is crucial in re-operative fields for assessing pedicle viability. In Hirschsprung disease, ICG-F assesses visualizing colonic derotation and selecting vessels for division57. Clinical findings in adult colorectal surgeries demonstrate that ICG-F enhances surgical quality and reduces complications98. While one must be cautious extrapolating findings to pediatrics, ICG-F was demonstrated as safe and feasible in intestinal resections, with positive feedback from the surgical team, suggesting improved visualization and patient outcomes51. ICG-F has demonstrable efficacy in enhancing surgical visualization and decision-making in pediatric colorectal and pelvic reconstructive surgeries for viability of bowel pedicles and anastomotic perfusion. Extrapolation from adult data suggests similar benefits in pediatric settings, however, this requires more validation.
Pediatric Urological Surgeries and the Role of ICG-F
Ten studies examined the utility of ICG-F in pediatric urological procedures13,35,56,67,69,71,83,99,100. ICG-F was employed in lymphatic sparring varicocele repairs, various renal surgeries (partial and total nephrectomies and renal cyst unroofing), ureteral mapping, and evaluating vascular and tissue perfusion for living-donor kidney transplantation. It has also been utilized in complex duplex renal surgeries, retroperitoneal lymph node dissections, and to define the ureter during tumor resections (ICG-F applied cystoscopically). Esposito et al. (2020)69 detailed 57 urological procedures, including 41 varicocele repairs featuring intraoperative lymphography and 16 renal surgeries. Intravenous injection of ICG was used for renal procedures, whereas intra-testicular injection was employed for varicocele repairs, resulting in visualization within 30-60 seconds after injection. The study confirmed ICG as a reliable tool for improving visualization in pediatric urology. ICG-F is a safe and effective tool for visualizing anatomical and vascular structures in pediatric urological surgeries. It proves essential for renal surgeries, ureteral mapping, and varicocele repairs with lymphography. Intravenous or intra-testicular ICG administration results in rapid visualization, enhancing surgery outcomes.
Pediatric Neurosurgical Applications of ICG-F
Ten studies examined ICG-F’s role in pediatric neurosurgical procedures15,30,44,45,58,60,60,80,82,85. ICG-F enhances the visualization and localization of cerebral lesions and maps vascular structures during operations, including tumor resections and arteriovenous malformation surgeries. Lehner et al. (2023)101 demonstrated ICG-F's ability to visualize the basilar artery during an endoscopic third ventriculostomy for an infant with congenital hydrocephalus. Horie et al. (2014)45 evaluate the utility of ICG video angiography (ICG-VA) in 50 patients to assess postoperative hyperperfusion in Moya Moya and atherosclerotic disease cases. They found that ICG-VA provides real-time cerebral blood flow data and helps identify patients at risk for postoperative hyperperfusion. Tanabe et al. (2017)82 studied 19 patients (8 pediatric) and demonstrated ICG-F’s efficacy in visualizing the middle meningeal artery before craniotomy for Moya Moya disease. ICG-F is an instrumental tool in pediatric neurosurgical applications, playing a significant role in enhancing visualization, delineating cerebral and vascular structures, and tissue perfusion. The technology demonstrates utility in intraoperative applications, contributing significantly to the safety and efficacy of complex procedures. Evidence from prospective studies suggests that ICG-F can provide real-time information crucial for surgical decision-making in intricate vascular neurosurgical diseases like MMD.
Thoracic
Sixteen articles in the review discussed the utility of ICG-F in pediatric thoracic surgery11,13,16,18–22,28,31–34,81,102,103 covering thoracoscopic tracheoesophageal fistula surgery, tumor resections, lung metastasectomies, and congenital cardiac surgery, thoracoscopic vascular ring surgery, and thoracoscopic repair of chylothorax. A prospective study by Abdelhafeez et al. (2023)14 investigated ICG-F’s efficacy in localizing metastatic pulmonary nodules in pediatric patients with solid tumors. Of the 50 patients with a total of 63 pulmonary nodules, ICG-F accurately detected 75% of positive nodules, falling short of the 90% accuracy goal. Notably, while pre-operative CT missed 26% of nodules linked to primary liver tumors, ICG-F was sensitive to them. The study advocated for further ICG-focused trials and measured use of ICG-F based on tumor histology. The study also suggested the cautious application of ICG-F imaging in patients with non-hepatic tumor metastases, depending on the tumor histology. ICG-F has demonstrated utility in many pediatric thoracic surgical interventions. ICG-F has a 75% accuracy for metastatic pulmonary nodules, without meeting the predefined target accuracy rate of 90%, but picks up 26% of preoperative CT missed nodules from hepatic solid tumors.
We recommend ICG-F, which has shown promise in various applications in pediatric thoracic surgery. However, its limitations in the context of nodule detection indicate a need for further prospective clinical trials using accepted standards for assessment and validation. The most reliable is solid hepatic tumor metastasis.
Additional Surgical Applications of ICG-F
The utility of ICG-F has been reported in various other surgical domains, including head and neck surgeries24,42,43, orthopedics36,38,39, endocrinological interventions, and plastic and reconstructive surgeries52. The limited breadth of the literature presents a pressing need for more research to assess the efficacy and safety of ICG-F in these surgical fields.
ICG-F dosing: Current Landscape and Challenges
Considerable variations in ICG-F dosing protocols emphasizing the absence of uniform reporting standards. According to the product guidelines from a recognized ICG distributor[1], the following maximum daily dosing parameters are recommended: Adults and Elderly: Up to 5 mg/kg of body weight. Adolescents (11-18 years): Up to 5 mg/kg of body weight. Children (2-11 years): Up to 2.5 mg/kg of body weight. Infants (0 months to 2 years): Up to 1.25 mg/kg of body weight.
However, most research articles advocate a more conservative daily dose of 0.6 mg/kg of ICG. A notable exception is the study by Abdelhafeez et al. (2022)104, which prescribes up to 1.5 mg/kg. Some use higher doses for non-liver lung metastasis of 4mg/kg. The optimal dosing standard protocols still need to be determined due to robust, evidence-driven research scarcity. The panel unanimously agrees that a weight-based dosing methodology appears most appropriate currently. However, ideal dosages may be contingent upon specific surgical procedures and individual patient characteristics.
Limitations
The consensus process highlighted several limitations: the diversity in study designs and lack of large-scale trials limit the strength of the evidence. Moreover, the variability in ICG-F dosing protocols across the literature points to the necessity for standardized guidelines. These limitations underline the preliminary nature of the consensus and the need for ongoing evaluation as further evidence emerges.
Conclusion
In summary, this consensus statement on ICG-F use in pediatric surgery aims to serve as a foundational reference that highlights its potential benefits. While promising, the current evidence remains scarce and calls for further investigation to establish comprehensive, evidence-based guidelines. The collective expert opinion, nevertheless, recognizes ICG-F as a valuable tool in pediatric surgical practice, with the potential to substantially elevate the standard of care.
Acknowledgements:
Keri Swaggart, Children’s Mercy – Kansas City Librarian
Marc Harms, Stryker Endoscopy, Stryker Nederland BV, Amsterdam, CM 1101, Netherlands.
Manuscript on behalf of the expert consensus group: Alex Bondoc, Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio, USA; Ciro Esposito, Federico II University Hospital, Naples, Italy; Seth D. Goldstein, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA; Grzegorz Kowalewski, Children's Memorial Health Institute, 04-730 Warsaw, Poland; Timothy B. Lautz, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA; Manuel Lopez, Val d'Hebron Maternity and Children's Hospital, Barcelona, Spain; Max Pachl, Birmingham Women's and Children's NHS Foundation Trust, University of Birmingham, UK; Samir Pandya, University of Texas Southwestern Medical Center, Dallas, Texas 75235, USA; Nelson Piché, Université de Montréal, Montréal, Québec, Canada ; Steven S. Rothenberg, Rocky Mountain Hospital for Children, Denver, CO 80205, USA; Jetske Ruiterkamp, Wilhelmina Children's Hospital, University Medical Center Utrecht, Utrecht, EA 3584, Netherlands; Stefan Scholz, UPMC Children's Hospital of Pittsburgh, University of Pittsburgh, Pittsburgh, Pennsylvania, USA; Benjamin Zendejas, Boston Children's Hospital, Boston, MA, USA.
The manuscript provided represents a shortened version of the original manuscript submitted to the Journal of Pediatric Surgery in January 2024 by Rebecca M. Rentea as corresponding author currently being under review and thus not representing an original article.
[1] https://diagnosticgreen.com/row/product-information/ [29.Sept.2023]
- Reinhart, M. B., Huntington, C. R., Blair, L. J., Heniford, B. T. & Augenstein, V. A. Indocyanine Green: Historical Context, Current Applications, and Future Considerations. Surg Innov 23, 166–175 (2016).
- Yannuzzi, L. A. Indocyanine Green Angiography: A Perspective on Use in the Clinical Setting. American Journal of Ophthalmology 151, 745-751.e1 (2011).
- Le-Nguyen, A. et al. The Use of Indocyanine Green Fluorescence Angiography in Pediatric Surgery: A Systematic Review and Narrative Analysis. Front. Pediatr. 9, 736242 (2021).
- Hamel, C. et al. Defining Rapid Reviews: a systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. Journal of Clinical Epidemiology 129, 74–85 (2021).
- Hamel, C. et al. Few evaluative studies exist examining rapid review methodology across stages of conduct: a systematic scoping review. Journal of Clinical Epidemiology 126, 131–140 (2020).
- Smela, B. et al. Rapid literature review: definition and methodology. Journal of Market Access & Health Policy 11, 2241234 (2023).
- Atkins D. Grading quality of evidence and strength of recommendations. BMJ 328, 1490 (2004).
- Meira, J., Marques, M. L., Falcão-Reis, F., Rebelo Gomes, E. & Carneiro, Â. Immediate Reactions to Fluorescein and Indocyanine Green in Retinal Angiography: Review of Literature and Proposal for Patient’s Evaluation. OPTH Volume 14, 171–178 (2020).
- Breuking, E. A. et al. Safety and Feasibility of Indocyanine Green Fluorescence Angiography in Pediatric Gastrointestinal Surgery: A Systematic Review. Journal of Pediatric Surgery 58, 1534–1542 (2023).
- Zeineddin, S. et al. Fluorescence-guided surgery: National trends in adoption and application in pediatric surgery. Journal of Pediatric Surgery 58, 689–694 (2023).
- Shirotsuki, R. et al. Novel thoracoscopic navigation surgery for neonatal chylothorax using indocyanine-green fluorescent lymphography. Journal of Pediatric Surgery 53, 1246–1249 (2018).
- Shibasaki, J. et al. Evaluation of Lymphatic Dysplasia in Patients with Congenital Pleural Effusion and Ascites Using Indocyanine Green Lymphography. The Journal of Pediatrics 164, 1116-1120.e1 (2014).
- Abdelhafeez, A. H. et al. Indocyanine green–guided nephron-sparing surgery for pediatric renal tumors. Journal of Pediatric Surgery 57, 174–178 (2022).
- Abdelhafeez, A. H. et al. Feasibility of indocyanine green‐guided localization of pulmonary nodules in children with solid tumors. Pediatric Blood & Cancer 70, e30437 (2023).
- Asayama, B. et al. Skull bone tumor resection with intraoperative indocyanine green fluorescence imaging: A series of four surgical cases. Interdisciplinary Neurosurgery 9, 8–13 (2017).
- Chen-Yoshikawa, T. F., Hatano, E., Yoshizawa, A. & Date, H. Clinical application of projection mapping technology for surgical resection of lung metastasis. Interactive CardioVascular and Thoracic Surgery 25, 1010–1011 (2017).
- Chung, P. H., Chok, K. S. & Wong, K. K. Indocyanine green fluorescence-assisted laparoscopic hepatectomy for hepatocellular carcinoma in a pre-adolescent girl: a case report. Hong Kong Med J 26, 342–344 (2020).
- Delgado‐Miguel, C., Estefanía, K., San Basilio, M. & Hernández Oliveros, F. Indocyanine green navigation in minimally invasive resection of multiple metachronous pulmonary metastases of hepatoblastoma. Thoracic Cancer 14, 528–532 (2023).
- Fung, C., Lau, C. & Wong, K. K. Indocyanine green fluorescence-guided pulmonary wedge resection in a child: a case report. Hong Kong Med J 26, 345–347 (2020).
- Harris, A. C., Choudhury, S. & Pachl, M. Early results of minimally invasive fluorescent guided pediatric oncology surgery with delivery of indocyanine green during induction of anesthesia. Photodiagnosis and Photodynamic Therapy 42, 103639 (2023).
- Kitagawa, N. et al. Navigation using indocyanine green fluorescence imaging for hepatoblastoma pulmonary metastases surgery. Pediatr Surg Int 31, 407–411 (2015).
- Komatsu, S. et al. Combined Use of Three-Dimensional Construction and Indocyanine Green-Fluorescent Imaging for Resection of Multiple Lung Metastases in Hepatoblastoma. Children 9, 376 (2022).
- Mitani, Y. et al. Real-time identification of hepatoblastoma using a near infrared imaging with indocyanine green. Journal of Pediatric Surgery Case Reports 2, 180–183 (2014).
- Richard, C. et al. Indocyanine green near infrared-guided surgery in children, adolescents, and young adults with otolaryngologic malignancies. Auris Nasus Larynx 50, 576–585 (2023).
- Shen, Q., Liu, X., Pan, S., Li, T. & Zhou, J. Effectiveness of indocyanine green fluorescence imaging in resection of hepatoblastoma. Pediatr Surg Int 39, 181 (2023).
- Shirota, C. et al. New Navigation Surgery for Resection of Lymphatic Malformations Using Indocyanine Green Fluorescence Imaging. Am J Case Rep 18, 529–531 (2017).
- Sound, S. et al. Intraoperative tumor localization and tissue distinction during robotic adrenalectomy using indocyanine green fluorescence imaging: a feasibility study. Surg Endosc 30, 657–662 (2016).
- Souzaki, R. et al. Navigation surgery using indocyanine green fluorescent imaging for hepatoblastoma patients. Pediatr Surg Int 35, 551–557 (2019).
- Takahashi, N. et al. Living Donor Liver Re-Transplantation for Recurrent Hepatoblastoma in the Liver Graft following Complete Eradication of Peritoneal Metastases under Indocyanine Green Fluorescence Imaging. Cancers 11, 730 (2019).
- Tsuzuki, S. et al. Application of indocyanine green (ICG) fluorescence for endoscopic biopsy of intraventricular tumors. Childs Nerv Syst 30, 723–726 (2014).
- Whitlock, R. S. et al. Pathologic correlation with near infrared-indocyanine green guided surgery for pediatric liver cancer. Journal of Pediatric Surgery 57, 700–710 (2022).
- Yamada, Y. et al. Fluorescence-Guided Surgery for Hepatoblastoma with Indocyanine Green. Cancers 11, 1215 (2019).
- Yamamichi, T. et al. Clinical application of indocyanine green (ICG) fluorescent imaging of hepatoblastoma. Journal of Pediatric Surgery 50, 833–836 (2015).
- Yoshida, M. et al. Clinicopathological study of surgery for pulmonary metastases of hepatoblastoma with indocyanine green fluorescent imaging. Pediatric Blood & Cancer 69, e29488 (2022).
- Arichi, N. et al. Intraoperative Fluorescence Vascular Imaging Using Indocyanine Green for Assessment of Transplanted Kidney Perfusion. Transplantation Proceedings 46, 342–345 (2014).
- Aung, T. et al. A novel indication for indocyanine green (ICG): Intraoperative monitoring of limb and sciatic nerve perfusion during rotationplasty for sarcoma patients. CH 70, 441–447 (2019).
- Castro-e-Silva, O. et al. Autofluorescence Spectroscopy in Liver Transplantation: Preliminary Results From a Pilot Clinical Study. Transplantation Proceedings 40, 722–725 (2008).
- Cleveland, C. A., Abdelgawad, A., Cook, J. & Pirela-Cruz, M. Use of Indocyanine Green Fluorescent Dye Video Angiography in Orthopaedic Trauma: A Pilot Study. J Surg Orthop Adv 22, 310–315 (2013).
- Connolly, P. H., Meltzer, A. J., Spector, J. A. & Schneider, D. B. Indocyanine Green Angiography Aids in Prediction of Limb Salvage in Vascular Trauma. Annals of Vascular Surgery 29, 1453.e1-1453.e4 (2015).
- Fernández-Bautista, B., Mata, D. P., Parente, A., Pérez-Caballero, R. & De Agustín, J. C. First Experience with Fluorescence in Pediatric Laparoscopy. European J Pediatr Surg Rep 07, e43–e46 (2019).
- Figueroa, R. et al. Indocyanine green fluorescence imaging to evaluate graft perfusion during liver transplantation. HPB 21, 387–392 (2019).
- Fried, F. W. et al. Free Latissimus Dorsi Myocutaneous Flap in a 6-Month-Old Child for Reconstruction of a Temporal Fossa Defect After Teratoma Resection. Ann Plast Surg 82, 62–63 (2019).
- Hinchcliff, K. M., Yao, A. & Taub, P. J. Laser-Assisted Indocyanine Green Imaging to Assess Perfusion of Scalp Closure in an Infant. Journal of Craniofacial Surgery 24, 2004–2006 (2013).
- Hori, S. et al. Surgical anatomy and preservation of the middle meningeal artery during bypass surgery for moyamoya disease. Acta Neurochir 157, 29–36 (2015).
- Horie, N. et al. Indocyanine green videoangiography for assessment of postoperative hyperperfusion in moyamoya disease. Acta Neurochir 156, 919–926 (2014).
- Iinuma, Y. et al. Intraoperative near-infrared indocyanine green fluorescence angiography (NIR-ICG AG) can predict delayed small bowel stricture after ischemic intestinal injury: Report of a case. Journal of Pediatric Surgery 48, 1123–1128 (2013).
- Ishikawa, K. et al. Preliminary Experience With Intraoperative Near-infrared Fluorescence Imaging in Percutaneous Sclerotherapy of Soft-Tissue Venous Malformations. Dermatologic Surgery 39, 907–912 (2013).
- Kaneshi, Y., Shibasaki, J., Aida, N., Shimokaze, T. & Toyoshima, K. Indocyanine green lymphography for congenital lymphatic dysplasia with tuberous sclerosis complex: A case report. Pediatrics International 62, 234–236 (2020).
- Kato, M., Watanabe, S., Iida, T., Watanabe, A. & Megumi, F. Peri-orbital lymphangioma treated by lymphatic-venous anastomosis with indocyanine green lymphography analysis. Journal of Pediatric Surgery Case Reports 23, 9–14 (2017).
- Kisaoglu, A., Demiryilmaz, I., Dandin, O., Ozkan, O. & Aydinli, B. Management of reperfusion deficiency with indocyanine green fluorescence imaging during deceased donor liver transplantation in a pediatric recipient. HPB 22, 633 (2020).
- Le-Nguyen, A. et al. Indocyanine green fluorescence angiography in pediatric intestinal resections: A first prospective mixed methods clinical trial. Journal of Pediatric Surgery 58, 82–88 (2023).
- Martins, D. B. et al. Intraoperative Indocyanine Green Laser Angiography in Pediatric Autologous Ear Reconstruction. Plastic and Reconstructive Surgery - Global Open 4, e709 (2016).
- Meisner, J. W. et al. Qualitative features of esophageal fluorescence angiography and anastomotic outcomes in children. Journal of Pediatric Surgery 58, 1359–1367 (2023).
- Numanoglu, A. & Millar, A. J. W. Necrotizing enterocolitis: Early conventional and fluorescein laparoscopic assessment. Journal of Pediatric Surgery 46, 348–351 (2011).
- Onishi, S. et al. Feasibility of delayed anastomosis for long gap esophageal atresia in the neonatal period using internal traction and indocyanine green‐guided near‐infrared fluorescence. Asian J Endoscop Surgery 15, 877–881 (2022).
- Paraboschi, I. et al. Indocyanine Green (ICG)-Guided Onlay Preputial Island Flap Urethroplasty for the Single-Stage Repair of Hypospadias in Children: A Case Report. IJERPH 20, 6246 (2023).
- Rentea, R. M. et al. Preliminary Use of Indocyanine Green Fluorescence Angiography and Value in Predicting the Vascular Supply of Tissues Needed to Perform Cloacal, Anorectal Malformation, and Hirschsprung Reconstructions. Eur J Pediatr Surg 30, 505–511 (2020).
- Sugimoto, T. et al. Effectiveness of intraoperative indocyanine green videoangiography in direct surgical treatment of pediatric intracranial pial arteriovenous fistula. PED 15, 55–59 (2015).
- Sugita, K. et al. A safe and effective laparoscopic Ladd’s procedure technique involving the confirmation of mesenteric vascular perfusion by fluorescence imaging using indocyanine green: A case report of an infant. Asian J Endoscop Surgery 15, 410–414 (2022).
- Takagi, Y., Sawamura, K., Hashimoto, N. & Miyamoto, S. Evaluation of Serial Intraoperative Surgical Microscope-Integrated Intraoperative Near-Infrared Indocyanine Green Videoangiography in Patients With Cerebral Arteriovenous Malformations. Operative Neurosurgery 70, ons34–ons43 (2012).
- Tomioka, Y. K., Narushima, M., Yamashita, S., Ito, A. & Okazaki, M. Foot Web Space Transfer for Congenital Syndactyly. Plastic and Reconstructive Surgery - Global Open 8, e3292 (2020).
- Vogt, P., Bauer, E. & Graves, K. Novadaq Spy TM Intraoperative Imaging System - Current Status. Thorac cardiovasc Surg 51, 49–51 (2003).
- Yada, K., Migita, M., Nakamura, R., Abe, S. & Matsufuji, H. Indocyanine green fluorescence during pediatric stoma closure. Journal of Pediatric Surgery Case Reports 61, 101595 (2020).
- Bada-Bosch, I. et al. Laparoscopic Partial Splenectomy Assisted by Fluorescence in a 13-Year-Old Girl. European J Pediatr Surg Rep 08, e81–e85 (2020).
- Bryant, M. K., Marulanda, K. & Phillips, M. R. Laparoscopic Double Cholecystectomy in a Pediatric Patient for Gallbladder Duplication: An Unusual Case of Biliary Anatomy. The American Surgeon 86, 1531–1534 (2020).
- Calabro, K. A., Harmon, C. M. & Vali, K. Fluorescent Cholangiography in Laparoscopic Cholecystectomy and the Use in Pediatric Patients. Journal of Laparoendoscopic & Advanced Surgical Techniques 30, 586–589 (2020).
- Esposito, C. et al. Indocyanine Green Fluorescence Lymphography: A New Technique to Perform Lymphatic Sparing Laparoscopic Palomo Varicocelectomy in Children. Journal of Laparoendoscopic & Advanced Surgical Techniques 29, 564–567 (2019).
- Esposito, C. et al. Laparoscopic or Robotic Deroofing Guided by Indocyanine Green Fluorescence and Perirenal Fat Tissue Wadding Technique of Pediatric Simple Renal Cysts. Journal of Laparoendoscopic & Advanced Surgical Techniques 30, 471–476 (2020).
- Esposito, C. et al. Near-Infrared fluorescence imaging using indocyanine green (ICG): Emerging applications in pediatric urology. Journal of Pediatric Urology 16, 700–707 (2020).
- Esposito, C. et al. Indocyanine green (ICG) fluorescent cholangiography during laparoscopic cholecystectomy using RUBINATM technology: preliminary experience in two pediatric surgery centers. Surg Endosc 35, 6366–6373 (2021).
- Esposito, C. et al. Technical standardization of ICG near-infrared fluorescence (NIRF) laparoscopic partial nephrectomy for duplex kidney in pediatric patients. World J Urol 39, 4167–4173 (2021).
- Esposito, C., Settimi, A., Cerulo, M. & Escolino, M. Efficacy of indocyanine green (ICG) fluorescent cholangiography to improve intra-operative visualization during laparoscopic cholecystectomy in pediatric patients: a comparative study between ICG-guided fluorescence and standard technique. Surg Endosc 36, 4369–4375 (2022).
- Graves, C., Ely, S., Idowu, O., Newton, C. & Kim, S. Direct Gallbladder Indocyanine Green Injection Fluorescence Cholangiography During Laparoscopic Cholecystectomy. Journal of Laparoendoscopic & Advanced Surgical Techniques 27, 1069–1073 (2017).
- Hirayama, Y. et al. Near-infrared fluorescence cholangiography with indocyanine green for biliary atresia. Real-time imaging during the Kasai procedure: a pilot study. Pediatr Surg Int 31, 1177–1182 (2015).
- Kobayashi, Y. et al. Portal vein territory identification using indocyanine green fluorescence imaging: Technical details and short-term outcomes. J Surg Oncol 116, 921–931 (2017).
- Kogon, B. et al. The Role of Intraoperative Indocyanine Green Fluorescence Angiography in Pediatric Cardiac Surgery. The Annals of Thoracic Surgery 88, 632–636 (2009).
- Lemoine, C. P., Lautz, T. B. & Superina, R. Indocyanine green fluorescence imaging as an adjunct for the localization of a bile leak after split liver transplantation. Pediatric Transplantation 27, e14431 (2023).
- Masuya, R. et al. Laparoscopic dome resection for pediatric nonparasitic huge splenic cyst safely performed using indocyanine green fluorescence and percutaneous needle grasper. Asian J Endoscop Surgery 15, 693–696 (2022).
- Mayorga-Buiza, M. J., Rivero-Garvia, M. & Márquez-Rivas, J. Microvascular Fluorescence in Spinal Cord Repair. World Neurosurgery 125, 245–246 (2019).
- Pandey, P., Ambekar, S., Babu, A. & Devi, I. Intraoperative assessment of STA-MCA bypass patency using near-infrared indocyanine green video-angiography: A preliminary study. Neurol India 60, 604 (2012).
- Pourmoghadam, K. K., Bunnell, A. P. M., O’Brien, M. C. & DeCampli, W. M. Avoiding Coronary Injury in Congenital Heart Surgery by Laser-Assisted Indocyanine Green Dye Imaging. World J Pediatr Congenit Heart Surg 5, 326–329 (2014).
- Tanabe, N. et al. Indocyanine green visualization of middle meningeal artery before craniotomy during surgical revascularization for moyamoya disease. Acta Neurochir 159, 567–575 (2017).
- Tomita, K. et al. Indocyanine Green Angiography-assisted Laparoendoscopic Single-site Varicocelectomy. Urology 106, 221–225 (2017).
- Troisi, R. I., Elsheikh, Y. M., Shagrani, M. A. & Broering, D. First fully laparoscopic donor hepatectomy for pediatric liver transplantation using the indocyanine green near-infrared fluorescence imaging in the Middle East: a case report. Annals of Saudi Medicine 34, 354–357 (2014).
- Ueba, T., Abe, H., Matsumoto, J., Higashi, T. & Inoue, T. Efficacy of indocyanine green videography and real-time evaluation by FLOW 800 in the resection of a spinal cord hemangioblastoma in a child: Case report. PED 9, 428–431 (2012).
- Yanagi, Y. et al. The outcome of real-time evaluation of biliary flow using near-infrared fluorescence cholangiography with Indocyanine green in biliary atresia surgery. Journal of Pediatric Surgery 54, 2574–2578 (2019).
- Esposito, C. et al. Image-Guided Pediatric Surgery Using Indocyanine Green (ICG) Fluorescence in Laparoscopic and Robotic Surgery. Front. Pediatr. 8, 314 (2020).
- Cheng, M. & Liu, T. T. Lymphedema microsurgery improved outcomes of pediatric primary extremity lymphedema. Microsurgery 40, 766–775 (2020).
- Drobot, A. et al. Resection of an axillary macrocystic lymphatic malformation in a 14-year-old girl using intraoperative indocyanine green lymphography. Journal of Vascular Surgery: Venous and Lymphatic Disorders 9, 504–507 (2021).
- Greives, M. R., Aldrich, M. B., Sevick-Muraca, E. M. & Rasmussen, J. C. Near-Infrared Fluorescence Lymphatic Imaging of a Toddler With Congenital Lymphedema. Pediatrics 139, e20154456 (2017).
- Jeremiasse, B. et al. ASO Visual Abstract: Sentinel Lymph Node Procedure in Pediatric Patients with Melanoma, Squamous Cell Carcinoma or Sarcoma Using Near-Infrared Fluorescence Imaging with Indocyanine Green: A Feasibility Trial. Ann Surg Oncol 30, 2399–2400 (2023).
- Kato, M., Watanabe, S., Iida, T. & Watanabe, A. Flow Pattern Classification in Lymphatic Malformations by Indocyanine Green Lymphography. Plastic & Reconstructive Surgery 143, 558e–564e (2019).
- Mansfield, S. A. et al. Alternative approaches to retroperitoneal lymph node dissection for paratesticular rhabdomyosarcoma. Journal of Pediatric Surgery 55, 2677–2681 (2020).
- Mihara, M. et al. Indocyanine Green Lymphography and Lymphaticovenous Anastomosis for Generalized Lymphatic Dysplasia with Pleural Effusion and Ascites in Neonates. Annals of Vascular Surgery 29, 1111–1122 (2015).
- Ogata, F. et al. Intraoperative Lymphography Using Indocyanine Green Dye for Near-Infrared Fluorescence Labeling in Lymphedema. Annals of Plastic Surgery 59, 180–184 (2007).
- Otake, K. et al. Use of computed tomography-lymphangiography with direct injection of water-soluble contrast medium to identify the origin of chylous ascites. Journal of Vascular Surgery: Venous and Lymphatic Disorders 3, 90–93 (2015).
- Tan, I.-C. et al. Investigational Lymphatic Imaging at the Bedside in a Pediatric Postoperative Chylothorax Patient. Pediatr Cardiol 35, 1295–1300 (2014).
- Safiejko, K. et al. Safety and Efficacy of Indocyanine Green in Colorectal Cancer Surgery: A Systematic Review and Meta-Analysis of 11,047 Patients. Cancers 14, 1036 (2022).
- Herz, D., DaJusta, D., Ching, C. & McLeod, D. Segmental arterial mapping during pediatric robot-assisted laparoscopic heminephrectomy: A descriptive series. Journal of Pediatric Urology 12, 266.e1-266.e6 (2016).
- Pachl, M. J. Fluorescent Guided Lymph Node Harvest in Laparoscopic Wilms Nephroureterectomy. Urology 158, 189–192 (2021).
- Lehner, M., Esslinger, P. & Szavay, P. A surgical first: Application of indocyanine green fluorescence imaging for endoscopic third ventriculostomy in an infant. Research Square (preprint) (2023) doi:10.21203/rs.3.rs-2830664/v1.
- Chang, T.-I., Chen, Y.-S. & Huang, S.-C. Intraoperative indocyanine green fluorescence lymphography to detect chylous leakage sites after congenital heart surgery. The Journal of Thoracic and Cardiovascular Surgery 148, 739–740 (2014).
- Pham, K. T. et al. Multimodality lymphatic imaging of postoperative chylothorax in an infant with Noonan syndrome: a case report. Eur J Med Res 25, 55 (2020).
- Abdelhafeez, A. H., Davidoff, A. M., Murphy, A. J., Arul, G. S. & Pachl, M. J. Fluorescence-guided lymph node sampling is feasible during up-front or delayed nephrectomy for Wilms tumor. Journal of Pediatric Surgery 57, 920–925 (2022).
- Ott, K. C. et al. Use of Near Infrared Ureteral Stent Fibers for Neonatal Colorectal Operations. Surg Innov 29, 550–551 (2022).
- Predina, J. D., Newton, A., Deshpande, C., Low, P. & Singhal, S. Utilization of targeted near-infrared molecular imaging to improve pulmonary metastasectomy of osteosarcomas. J. Biomed. Opt. 23, 1 (2018).